 Bookmark
Bookmark Top Health Challenges for Men and Women
Top Health Challenges for Men and Women
Women and men face many of the same health challenges including heart disease, stroke, cancers, and diabetes. However, some conditions are unique to men or women. Underlying biological differences, genetic contributions, sex hormones, and other factors dictate the response to an exposure and sensitivity to an exposure or treatment, which culminates in a different risk of developing certain diseases for men and women.1
Health Challenges for Women
Several conditions that are unique to women include those related to the organs of their reproductive system. For example, polycystic ovarian syndrome and endometriosis affect the ovaries and endometrial tissue of the uterine cavity, respectively.2,3 Both conditions, along with other reproductive conditions, can impose a heavy burden on women and have long-term effects.2,3
Lung conditions also affect women more often than men, including increased risk and worse severity and mortality.1 These conditions include asthma, chronic obstructive pulmonary disease (COPD), pulmonary hypertension, and some forms of lung cancer.1 Women with COPD also display different symptoms than men with COPD; the prevalence of COPD is also increasing at a faster rate in women than in men.1 Additionally, the odds of developing major lung cancer are higher in women than men at every level of cigarette smoke exposure, indicating women have increased sensitivity to the carcinogens found in tobacco.1
Additionally, women are:
- At a higher risk for breast cancer4
- More likely to show signs of stress, depression, and anxiety, as well as be diagnosed with depression4,5
- At a greater risk of developing Alzheimer’s disease, even after accounting for generally increased lifespan and experience significantly faster decline and greater deterioration than men of the same age4
- More likely to suffer from autoimmune diseases including multiple sclerosis and celiac disease5,6
- More likely to die from diabetes7
Women are also more likely than men to suffer a stroke although they share many of the same risk factors.4 Risk factors that are specific to women include the use of oral contraceptives, being pregnant, having frequent migraine headaches, as well as having a larger waist circumference.4
Health Challenges for Men
One of the biggest health concerns among men, especially men aged 80 or older, is prostate health, including benign prostatic hyperplasia and prostate cancer. Prostate cancer is the second most diagnosed type of cancer and risk factors include age, obesity, family history, and ethnicity.8 Benign prostatic hyperplasia (BPH) is not a form of cancer, although the prostate gland becomes enlarged and obstructs bladder output; it can lead to issues in the urinary tract and decrease the quality of life.9
Males also experience an increased burden of:10
- Autism spectrum disorder, specifically in school-aged boys
- Developing Parkinson’s disease
- Ulcerative colitis after age 45
- Psychotic disorders under the age of 40
Nuances in Disease Risk
Studying the risk of diseases over time, as well as sex-based differences in severity and outcomes can be challenging. For example, men are more likely to become dependent on or addicted to alcohol, but the effects of alcohol abuse are more significant in women.4 Similarly, the incidence of sexually transmitted infections is similar, but the consequences can be more serious in women because they are more likely to go unnoticed or dismissed and therefore untreated.4 Another complicating factor is age, as disease risk can change throughout the lifespan, especially with a shift being observed during puberty. Puberty and the associated changes in sex hormones change the trends for some conditions including obstructive sleep apnea which is similarly pervasive among young boys and girls, but becomes more prevalent in boys after puberty.1
Mechanisms Underlying Differences in Disease Burden
Biological differences between men and women, including anatomy, sex hormones, genetic and epigenetic differences, and other socioeconomic, cultural, and environmental exposures all play a role in the unique disease burden experienced by men and women.6 Reproductive load may also alter the risk of developing diseases for women as estrogen interacts with immune cells.6
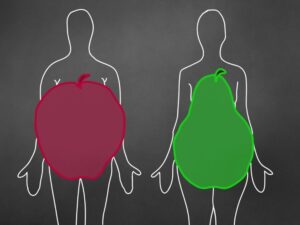
Differences in outcomes related to metabolic diseases have been partially attributed to body shape. Whereas women typically demonstrate a pear shape with more subcutaneous fat, men tend to have an apple shape with visceral fat lining the abdominal organs.11 Abdominal fat correlates strongly with increased risk of metabolic complications, while lower body fat is associated with a reduced risk and may be protective.11
Supporting Health in Both Men and Women
There are strategies both women and men can develop to decrease the risk of certain diseases over their lifetime. Consuming a balanced diet that is full of nutrient-dense foods, low in processed foods and refined sugars, and high in lean protein and healthy fats provides many benefits to the body, including lowering the risk of metabolic disorders. Additionally, including “brain-healthy” foods such as salmon, nuts, and blueberries can help support cognitive health. Ensuring adequate intake of essential nutrients, vitamins, and minerals can also help the body function at its optimal capacity and protect cells from damage. Finally, maintaining healthy habits around sleep, hydration, and physical activity can help protect from both acute and chronic diseases.
Men and women face shared and sex-specific health challenges. However, reducing the risk of developing a disease down to a single variable, including sex, can over-simplify the complex pathogenesis of diseases. There are also other differences between men and women that may alter disease risk or outcome and can be difficult to quantify and study. Consuming a healthy diet and seeking treatment for symptoms, regardless of sex, can help decrease the risk of many health challenges.
References
- Silveyra, P., Fuentes, N., Bauza, D.R. (2021). Sex and Gender Differences in Lung Disease. Adv Exp Med Biol, 1304:227-258.
- Gadalla, M.A., Norman, R.J., Tay, C.T., Hiam, D.S., Melder, A., Pundir, J., Thangaratinam, S., Teede, H.J., Mol, B.W.J., Moran, L.J. (2020). Medical and Surgical Treatment of Reproductive Outcomes in Polycystic Ovary Syndrome: An Overview of Systematic Reviews. Int J Fertil Steril, 13(4):257-270.
- Della Corte, L., Di Filippo, C., Gabrielli, O., Reppuccia, S., La Rosa, V.L., Ragusa, R., Fichera, M., Commodari, E., Bifulco, G., Giampaolino, P. (2020). The Burden of Endometriosis on Women’s Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int J Environ Res Public Health, 17(13):4683.
- (2016, December 1). What health issues or conditions affect women differently than men? Eunice Kennedy Shriver National Institute of Child Health and Human Development. What health issues or conditions affect women differently than men? | NICHD – Eunice Kennedy Shriver National Institute of Child Health and Human Development (nih.gov). Retrieved May 2022.
- Li, R., Singh, M. (2014). Sex Differences in Cognitive Impairment and Alzheimer’s Disease. Front Neuroendocrinol, 35(3):385-403.
- Ngo, S.T., Steyn, F.J., McCombe, P.A. (2014). Gender differences in autoimmune disease. Front Neuroendocrinol, 35(3):347-369.
- de Ritter, R., de Jong, M., Vos, R.C., van der Kallen, C.J.H., Sep, S.J.S., Woodward, M., Stehouwer, C.D.A., Bots, M.L., Peters, S.A.E. (2020). Sex differences in the risk of vascular disease associated with diabetes. Biol Sex Differ, 11(1):1-11.
- Termini, D., Hartogh, D.J.D., Jaglanian, A., Tsiani, E. (2020). Curcumin against Prostate Cancer: Current Evidence. Biomolecules, 10(11):1536-1575.
- Shore, N. (2015). A Review of the Prostatic Urethral Life for Lower Urinary Tract Symptoms: Symptom Relief, Flow Improvement, and Preservation of Sexual Function in Men With Benign Prostatic Hyperplasia. Curr Bladder Dysfunct Rep, 10(2):186-192.
- Holingue, C., Budavari, A.C., Rodriguez, K.M., Zisman, C.R., Windheim, G., Fallin, M.D. (2020). Sex Differences in the Gut-Brain Axis: Implications for Mental Health. Curr Psychiatry Rep, 22(12):83.
- Chang, E., Varghese, M., Singer, K. (2019). Gender and Sex Differences in Adipose Tissue. Curr Diab Rep, 18(9):69.
- Silveyra, P., Fuentes, N., Bauza, D.R. (2021). Sex and Gender Differences in Lung Disease. Adv Exp Med Biol, 1304:227-258.
- Gadalla, M.A., Norman, R.J., Tay, C.T., Hiam, D.S., Melder, A., Pundir, J., Thangaratinam, S., Teede, H.J., Mol, B.W.J., Moran, L.J. (2020). Medical and Surgical Treatment of Reproductive Outcomes in Polycystic Ovary Syndrome: An Overview of Systematic Reviews. Int J Fertil Steril, 13(4):257-270.
- Della Corte, L., Di Filippo, C., Gabrielli, O., Reppuccia, S., La Rosa, V.L., Ragusa, R., Fichera, M., Commodari, E., Bifulco, G., Giampaolino, P. (2020). The Burden of Endometriosis on Women’s Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int J Environ Res Public Health, 17(13):4683.
- (2016, December 1). What health issues or conditions affect women differently than men? Eunice Kennedy Shriver National Institute of Child Health and Human Development. What health issues or conditions affect women differently than men? | NICHD - Eunice Kennedy Shriver National Institute of Child Health and Human Development (nih.gov). Retrieved May 2022.
- Li, R., Singh, M. (2014). Sex Differences in Cognitive Impairment and Alzheimer’s Disease. Front Neuroendocrinol, 35(3):385-403.
- Ngo, S.T., Steyn, F.J., McCombe, P.A. (2014). Gender differences in autoimmune disease. Front Neuroendocrinol, 35(3):347-369.
- de Ritter, R., de Jong, M., Vos, R.C., van der Kallen, C.J.H., Sep, S.J.S., Woodward, M., Stehouwer, C.D.A., Bots, M.L., Peters, S.A.E. (2020). Sex differences in the risk of vascular disease associated with diabetes. Biol Sex Differ, 11(1):1-11.
- Termini, D., Hartogh, D.J.D., Jaglanian, A., Tsiani, E. (2020). Curcumin against Prostate Cancer: Current Evidence. Biomolecules, 10(11):1536-1575.
- Shore, N. (2015). A Review of the Prostatic Urethral Life for Lower Urinary Tract Symptoms: Symptom Relief, Flow Improvement, and Preservation of Sexual Function in Men With Benign Prostatic Hyperplasia. Curr Bladder Dysfunct Rep, 10(2):186-192.
- Holingue, C., Budavari, A.C., Rodriguez, K.M., Zisman, C.R., Windheim, G., Fallin, M.D. (2020). Sex Differences in the Gut-Brain Axis: Implications for Mental Health. Curr Psychiatry Rep, 22(12):83.
- Chang, E., Varghese, M., Singer, K. (2019). Gender and Sex Differences in Adipose Tissue. Curr Diab Rep, 18(9):69.











