Pro-inflammatory cytokines promote autoimmune inflammation and tissue damage, while anti-inflammatory cytokines help resolve inflammation and facilitate tissue repair.1 Macrophages, monocytes, and CD4+ T helper cells (Th1) produce tumor necrosis factor, which is a key driver of inflammation. Other pro-inflammatory cytokines include:
- Interferon ϒ
- Interleukin-1β
- Interleukin (IL)-6
- IL-17
A major mechanism of autoimmune disorders is an altered balance between the pathogenic T helper 17 (Th17) and protective regulatory T (Treg) cells. A shift toward Th17 promotes inflammat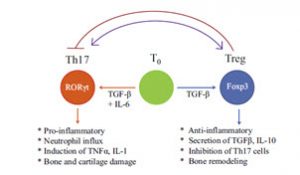 ion, neutrophil influx, induction of tumor necrosis factor alpha (TNFα), and joint damage in the case of rheumatoid arthritis (RA). This is an autoimmune condition characterized by chronic inflammation of the synovial tissue, joint dysfunction, and tissue damage in the joints. A shift towards Treg control promotes an anti-inflammatory tone. Perturbation of this balance can facilitate the induction and progression of autoimmune pathology.2
ion, neutrophil influx, induction of tumor necrosis factor alpha (TNFα), and joint damage in the case of rheumatoid arthritis (RA). This is an autoimmune condition characterized by chronic inflammation of the synovial tissue, joint dysfunction, and tissue damage in the joints. A shift towards Treg control promotes an anti-inflammatory tone. Perturbation of this balance can facilitate the induction and progression of autoimmune pathology.2
When the immune system attacks host tissue, the results can be devastating. There are many types of tissues and organs that can be impacted by autoimmune attack. The autoimmune attack can destroy the affected tissue and also negatively impact organ function. 3
Defective inflammation resolution is an underlying cause of prevalent chronic inflammatory diseases, such as atherosclerosis.4 Chronic inflammation is a failure to resolve inflammatory mediators leading to a chronic state of dysregulation. Resolvins involved in the acute phase of inflammation support resolution responses and the return to homeostasis. Importantly, pro-resolution pathways are not immunosuppressive. Dysregulation in resolving inflammation may be due to enzymatic insufficiency of the enzymes involved in converting long chain fatty acid metabolites to their oxidized derivatives that form the superfamily of pro-resolving mediators.5
Read part 5 of the Immune System Series: Nutrition is Essential for A Healthy Immune System.















