Bookmark
Bookmark Glucose Metabolism Hormones: Understanding Their Influence on Physiology
Glucose, a monosaccharide, provides fuel for cells in the body which enables organs to carry out essential functions efficiently. Through a series of reactions, glucose is converted to the cellular energy currency adenosine triphosphate (ATP), which fuels biochemical processes throughout the body including enzymatic reactions, substrate transport, and muscle contraction.
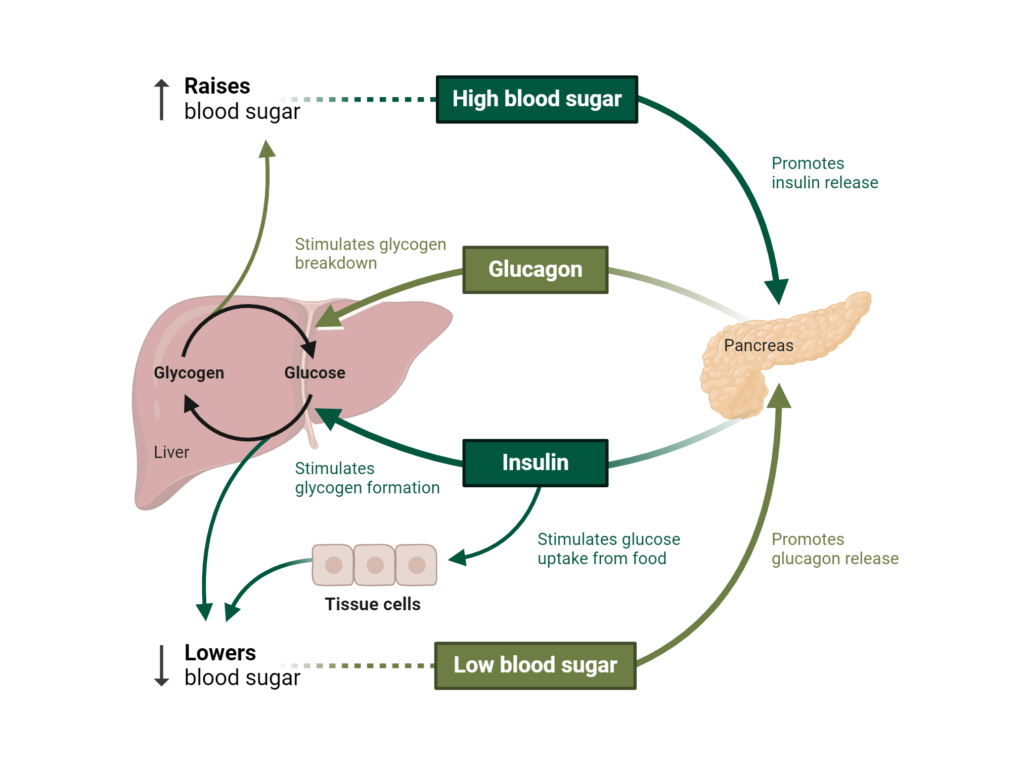
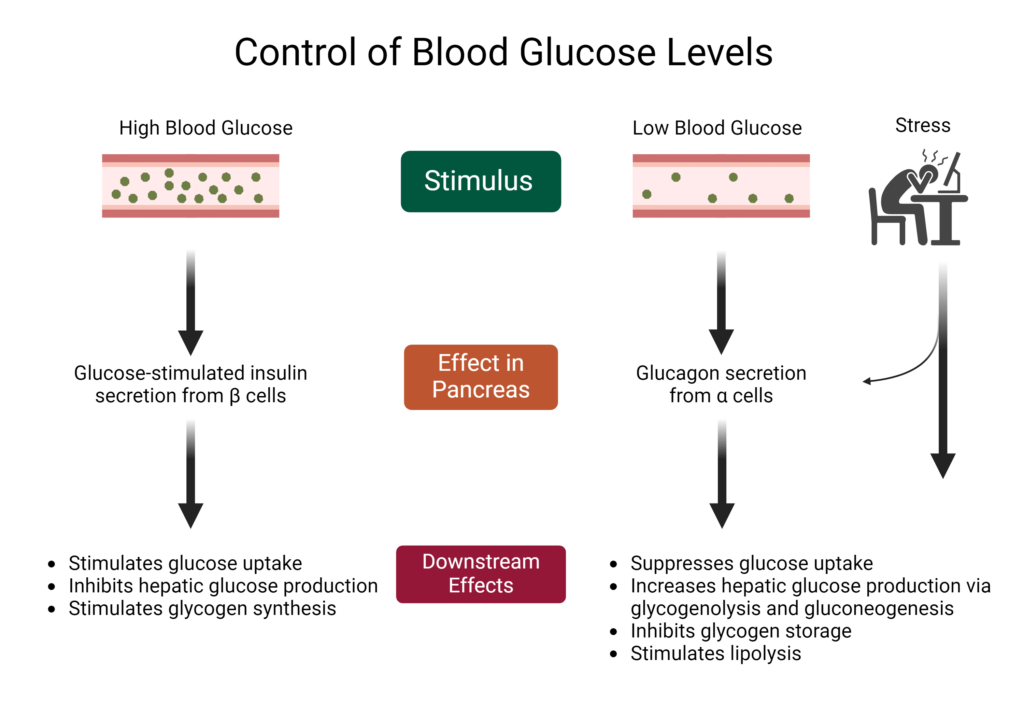
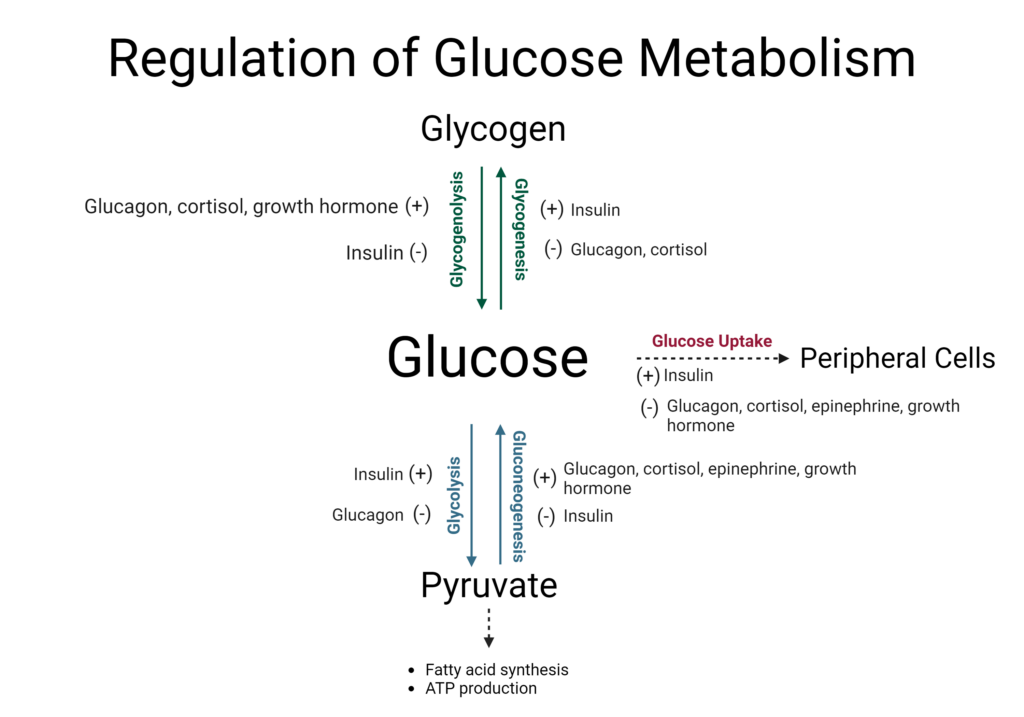
If blood glucose levels are too high or too low, it can impair essential functions in the body. To help keep blood glucose levels in an appropriate range, several hormones regulate glucose homeostasis. The major glucose-regulating hormones are insulin and glucagon; however, other hormones play a role in glucose homeostasis, including cortisol, epinephrine, and growth hormone.
Adapted from “Regulation of Blood Glucose”, by BioRender.com (CurrentYear). Retrieved from https://app.biorender.com/biorender-templates
Insulin
Insulin is a peptide hormone that functions as a key regulator of blood glucose levels. When the pancreas detects a rise in glucose concentration, insulin is released from pancreatic β-cells into the bloodstream and eventually signals cells to transport glucose from the bloodstream. Additionally, insulin acts as a growth-promoting signal, stimulating glycogen synthesis as a result of sufficient blood glucose. To avoid redundant cycles of glucose uptake and release, insulin inhibits glucagon secretion while promoting glucose uptake, glycogen synthesis, and signaling various growth factors.
In a state of insulin resistance, cells of the body become less sensitive to insulin signaling, requiring the pancreas to secrete more insulin to achieve the desired effect. In the short term, the pancreas can handle the increased load, however, over time, it can become exhausted and struggle to produce and secrete enough insulin to meet the increased demand. As a result, blood glucose levels remain elevated, resulting in hyperglycemia.
Eventually, this can lead to pre-diabetes and type 2 diabetes. Individuals with these conditions are encouraged to walk or engage in light exercise after consuming a glucose-containing meal to help the body take up glucose via insulin-independent pathways. In contrast to type 2 diabetes, type 1 diabetes is characterized by a lack of insulin production in the pancreas, and as a result, individuals with type 1 diabetes must receive insulin therapy to properly manage blood glucose levels.
Glucagon
Glucagon is a peptide hormone that directly opposes the actions of insulin. It is released from pancreatic α-cells when blood glucose levels are low, such as during an overnight fast or between meals, and in response to stress.1 When blood glucose levels are low, glucagon stimulates the liver to produce glucose via glycogenolysis, or the breakdown of glycogen. It also promotes gluconeogenesis to produce glucose from other substrates such as amino acids. Finally, glucagon inhibits glycogen synthesis, because the body is not equipped to store glycogen due to low blood glucose levels.
In some cases of hypoglycemia, glucagon is administered to raise blood glucose levels. However, clinical research has demonstrated a complex relationship between glucagon and downstream effects.1 For example, the effects of glucagon may differ between a fasted or postprandial state, and glucagon administration may also have unintended consequences on amino acid and lipid metabolism.1 Glucagon secretion can also become dysregulated in some metabolic conditions, including glucagon resistance in a state of obesity, although the prevalence and consequences of this effect in humans are not clear.1
Created with BioRender.com
Cortisol
Cortisol is a steroid hormone produced in the adrenal glands that coordinates the stress response in the body, including modulating glucose metabolism. Whereas insulin and glucagon act quickly, cortisol is a slower-acting hormone, which acts to maintain sufficient plasma glucose to provide to the brain during stress.2,3
The mechanisms through which cortisol affects glucose metabolism are complex, but at a broad level, cortisol counteracts insulin while increasing glucagon secretion via its effects on pancreatic β- and α-cells.2 In peripheral tissues, cortisol exhibits tissue-specific effects:2
- In the liver, cortisol promotes gluconeogenesis and decreases glycogen storage.
- In white adipose tissue cortisol decreases glucose uptake and utilization.
- In skeletal muscle cortisol increases the breakdown of glycogen in skeletal muscle to provide glucose for energy.
Cortisol helps maintain blood glucose levels during times of stress, synergizing the effects of glucagon, so essential organs have energy to carry out their functions.2 However, long-term stress can lead to chronically elevated cortisol and consequently altered insulin and glucagon signaling. Over time, this can contribute to insulin resistance as pancreatic β-cells attempt to compensate.
Eventually, β-cell hyperplasia and chronic hyperinsulinemia can impair β-cell function, leading to insufficient insulin secretion, hyperglycemia, and potentially type 2 diabetes.2 Managing cortisol levels through healthy diet, exercise, and stress management practices can help keep cortisol levels in a healthy range which, in turn, can support glucose homeostasis.
Epinephrine
Similar to cortisol, epinephrine, or adrenaline, is involved in the body’s stress response as well as maintaining glucose homeostasis. Epinephrine attempts to increase glucose concentration from energy stores, including fat, to prepare for physical activity or recover from hypoglycemia. To accomplish this, epinephrine must counteract and suppress the actions of insulin, including activating glucagon secretion.2,3 Epinephrine is a relatively fast-acting hormone, suppressing insulin secretion, stimulating the liver to produce glucose, and stimulating lipolysis to increase substrates for energy production while decreasing glucose utilization to spare glucose for vital functions.3
Created with BioRender.com
For individuals with adrenal conditions affecting epinephrine levels, proper management is essential for balancing hormone levels as well as maintaining glucose homeostasis. To support overall adrenal health, consistent consumption of nutrients from whole foods as well as certain herbs can provide important cofactors for hormone synthesis and support the body’s response to stress.
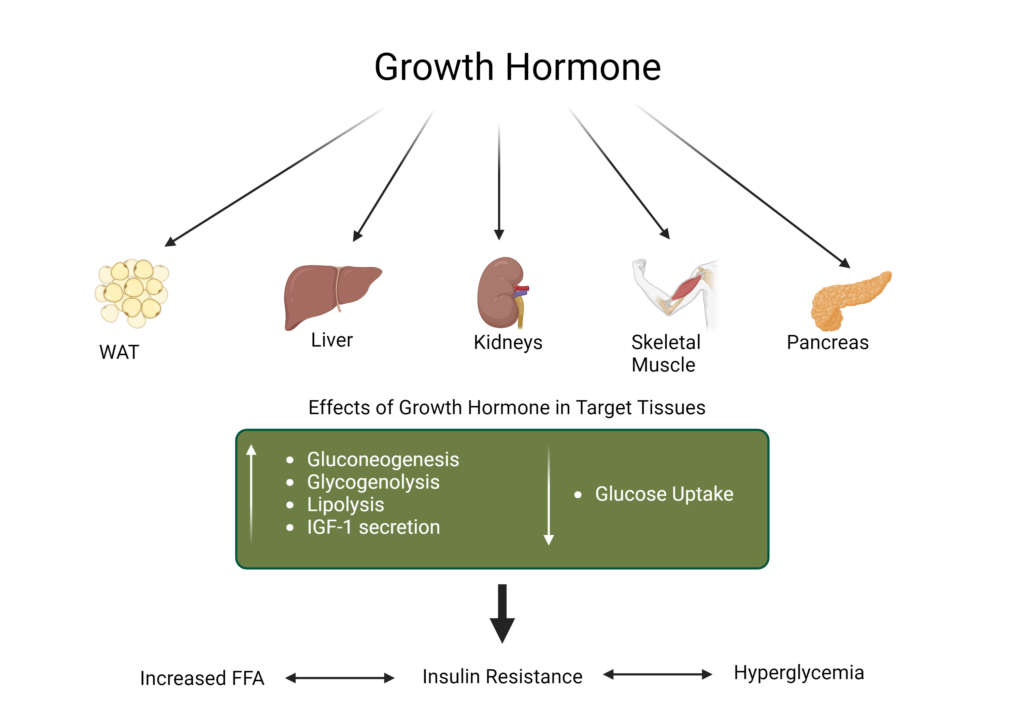
Growth Hormone
Growth hormone is released from the pituitary gland to promote growth in children, but in adults, it helps maintain glucose homeostasis.4 As a slow-acting growth signal, it stimulates protein synthesis and cell growth, while promoting lipolysis via the activation of hormone-sensitive lipase in adipose tissue to produce fatty acids for energy production.3,4
In relation to glucose metabolism, growth hormone exerts several direct effects, including increasing gluconeogenesis and glycogenolysis to produce more glucose in the liver and kidney, as well as counteracting insulin signaling and suppressing glucose uptake in some peripheral tissues, including white adipose tissue.4 Within the pancreas, growth hormone can directly promote β-cell proliferation, resulting in enhanced glucose-stimulated insulin secretion but in the long term, this can result in β-cell exhaustion and apoptosis, decreasing insulin secretion.4 Indirectly, growth hormone stimulates the production of insulin-like growth factor 1 (IGF-1), which lowers blood glucose.4
Created with BioRender.com
The complex effects of growth hormone can be seen in clinical conditions stemming from too much or too little growth hormone. For example, there is a high prevalence of diabetes in individuals with acromegaly, a condition in which excess growth hormone causes tissues and bones to grow too quickly.4 However, adults with a deficiency of growth hormone may also experience increased abdominal obesity, insulin resistance, dyslipidemia, and hyperglycemia.4
Treatment with growth hormone can help relieve these symptoms and restore homeostasis although there may be negative impacts on glucose homeostasis with growth hormone treatment, including impaired glucose tolerance and reduced insulin sensitivity.4
These five hormones, in addition to several others, regulate the complex network of glucose signaling and homeostasis. Insulin is the primary hormone response for lowering blood glucose levels while glucagon, epinephrine, cortisol, and growth hormone work as gluco-counter-regulatory hormones to raise blood glucose concentrations.
They can also enhance the effects of each other and are critical to maintaining sufficient blood glucose during the body’s stress response.5 This complex network of glucose regulation helps ensure healthy metabolism throughout the body and imbalances of one or multiple of these hormones can have serious detrimental effects.
- Janah, L., Kjeldsen, S., Galsgaard, K.D., Winther-Sorensen, M., Stojanovska, E., Pedersen, J., et al. (2019). Glucagon Receptor Signaling and Glucagon Resistance. Int J Mol Sci, 20:3314.
- Kuo, T., McQueen, A., Chen, T.-C., Wang, J.-C. (2015). Regulation of Glucose Homeostasis by Glucocorticoids. Adv Exp Med Biol, 872:99.
- Verberne, A.J.M, Korim, W.S., Sabetghadam, A., Llewellyn-Smith, I.J. (2016). Adrenaline: insights into its metabolic roles in hypoglycemia and diabetes. Br J Pharmacol, 173:1425.
- Kim, S.-H., Park, M.-J. (2017). Effects of growth hormone on glucose metabolism and insulin resistance in human. Ann Pediatr Endocrinol Metab, 22:145.
- Thau, L., Gandhi, J., Sharma, S. Physiology, Cortisol. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538239/.