About this PDF
Reducing pain and unresolved inflammation takes an integrative approach that both comprehensively evaluates and supports the patient with interventions such as nutrition. A useful framework is the “6 As” approach.
It is important to note obstacles that may impact a patient’s ability to make changes. Additionally, identifying behavioral and functional interventions will fully support the patient as they initiate a program.
According to data from a 2010 study, predictors of disabling chronic low back pain include:1
- Maladaptive pain coping behaviors, such as fear avoidance and catastrophizing
- Psychiatric comorbidities, such as depression and anxiety
- Functional impairment
- Poor general health status, including obesity, physical inactivity, smoking, and/or an inflammatory or nutrient-deficient diet
- Nonorganic signs, such as an overreaction to stimuli, non-reproducibility of pain, and/or superficial or nonanatomic tenderness
In some cases, if the obstacles are major, such as depression, it may be prudent to delay the program until behavioral and support interventions can help patients be in a setting where they can more fully engage in the program.
The 6 As
- Assess
Assess for underlying comorbidities and pain behaviors that will need attention to most significantly treat pain and reduce disability. Plus, assess for pain triggers in a stepwise fashion.
- Advise
Advise the patient on a stepwise strategy for reducing long-term pain and dispelling myths.
- Acknowledge
Acknowledge a patient’s fears and doubts.
- Activate
Motivate the patient for lifestyle change and stress the importance of self-care and empowerment to maximize an integrative approach focusing on the removal of triggers.
- Allow
Allow patient-centered decision making.
- Ally
Ally with the patient to maximize progress and reduce obstacles.
Nutritional Approaches to Pain Management
After comprehensive evaluation using the 6 As approach or another similar approach, integrative approaches can be individually initiated with shared decision making. Nutritional approaches move patients away from the Standard American Diet and focuses on the “Ps” and “Rs” of pain management, as in figure 1 and 2 below. These nutritional approaches are some of the most powerful for reducing pain as well as those that are often overlooked by patients and providers.
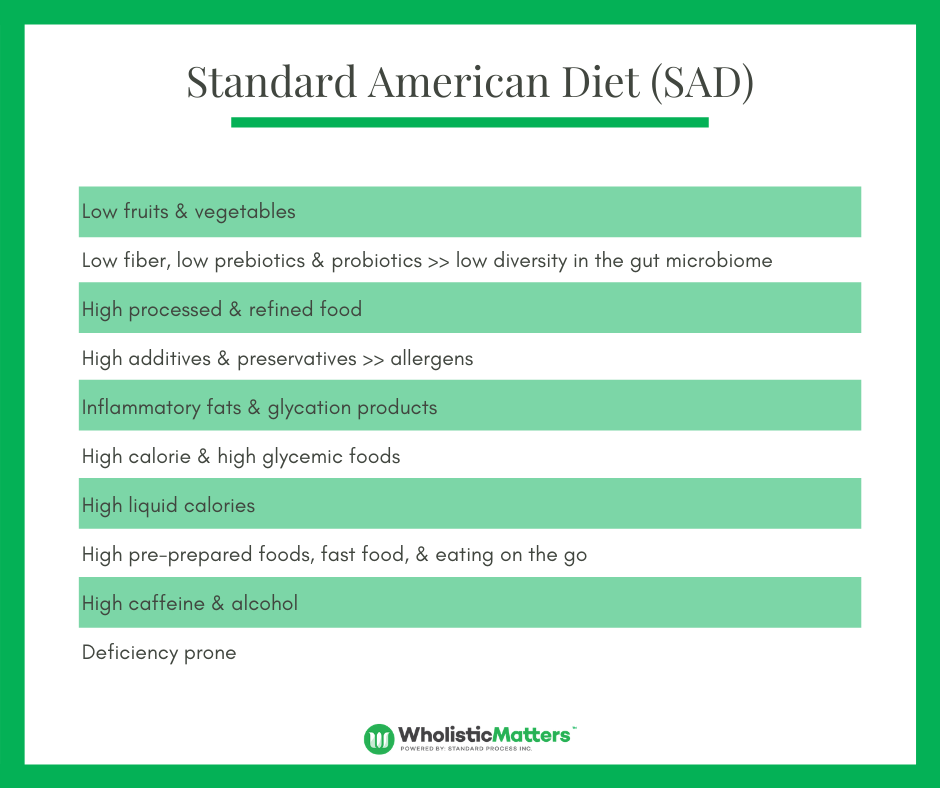
Figure 1: Hallmarks of the Standard American Diet (SAD)
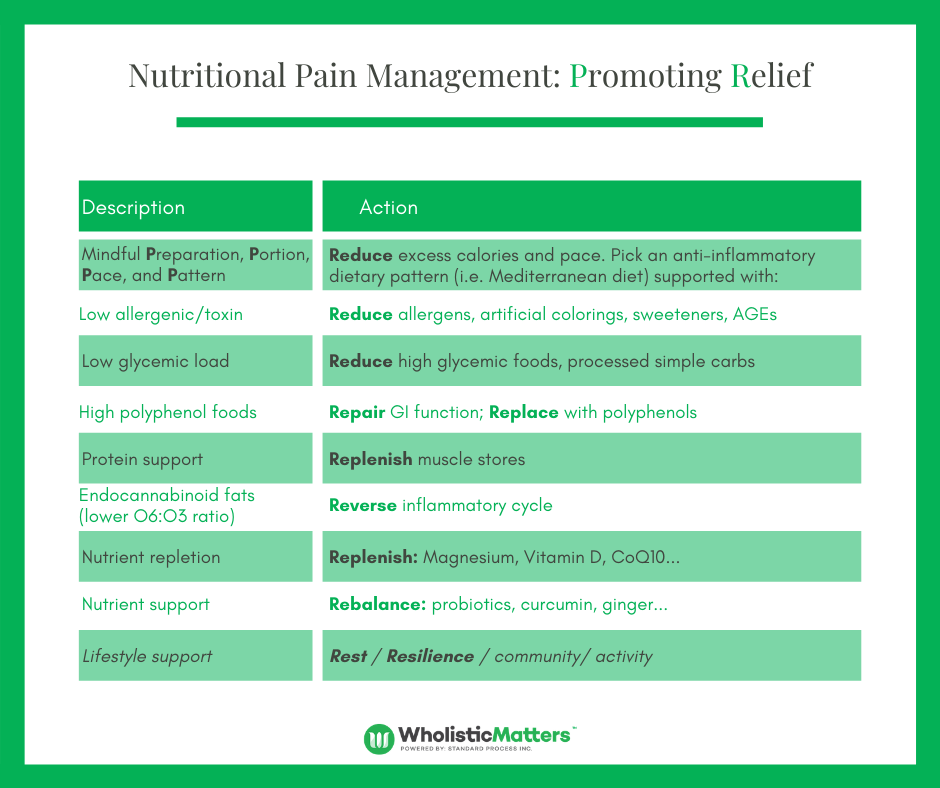
Figure 2: The Ps and Rs of Lifestyle Change
The first step before officially starting the program is Preparation. The Ps a practitioner should consider while preparing a patient for the program include:
Pre-testing: Lab testing for nutrient levels, inflammation, glucose, cholesterol, hormones, microbiome status, and other areas relevant to understanding the patient’s baseline status.
Purchasing: Encourage the patient to focus on low-toxin whole foods, organic when possible.
Reducing toxin exposure, including pesticides from food purchases, is one of the most impactful ways to reduce inflammation and improve health. Practitioners can encourage patients to make all purchases organic, especially when purchasing certain fruits and vegetables known to have the highest likelihood of elevated toxin levels. For example:
- More than 90 percent of samples of strawberries, apples, cherries, spinach, nectarines, and kale tested positive for residues of two or more pesticides.
- Multiple samples of kale showed 18 different pesticides.
- Kale and spinach samples had, on average, 1.1 to 1.8 times as much pesticide residue by weight than any other crop.2
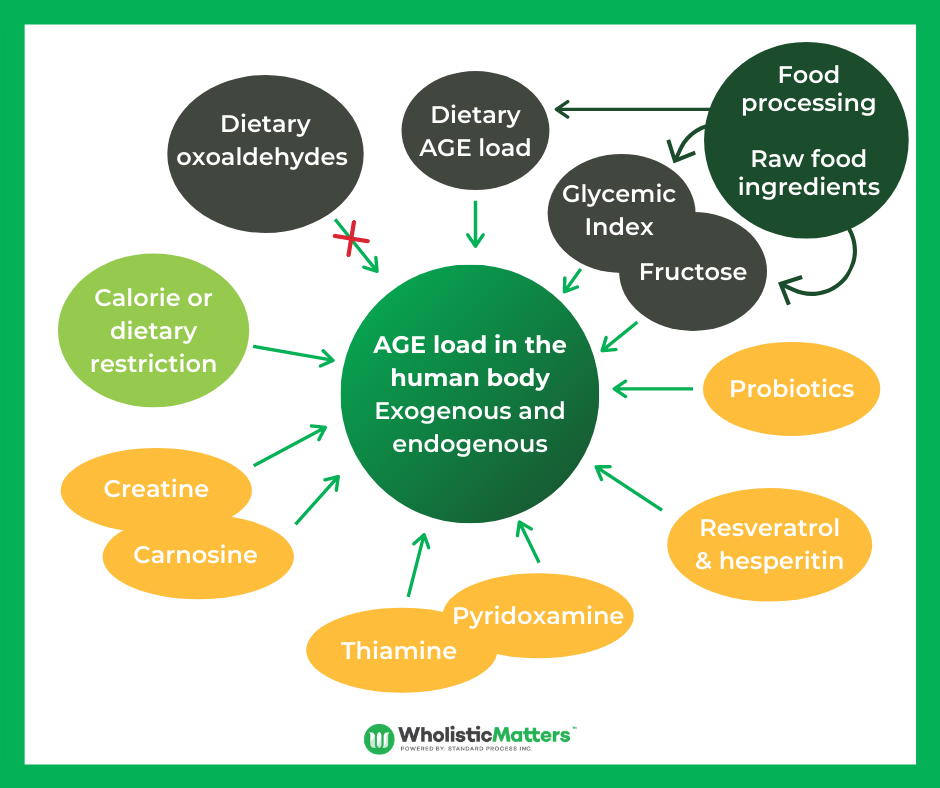
Preparing meals: The way food is prepared is intricately linked with the level of toxins present. During food preparation, it is important to avoid producing advanced glycation end products (AGEs). AGEs during cooking can be significantly reduced by:
- Cooking with moist heat
- Using shorter cooking times
- Cooking at lower temperatures
- Using acidic ingredients such as lemon juice or vinegar
Agents under research for AGE scavenging include aminoguanidine & Pyridoxamine.3
Pacing meals: Practitioners can encourage patients to consider mindful eating.
It is easy for patients to get into a pattern of eating too quickly. This is especially true for individuals in pain. Food intake can sometimes be with “quick hit” foods, consumed with not enough time to be aware of an individual’s food choices. Even with healthy foods, research shows that if individuals are not eating in a slow manner (i.e. taking at least 15 minutes – or more preferably 30 minutes or more) to finish a meal, this can cause increased inflammation even if the foods consumed are healthy. This is because it takes time for the digestive machinery to be ready to fully handle the caloric and nutrient load. By eating slowly, the enzymes and co-factors needed to fully digest food will have the appropriate time and ability to kick in and reduce any extra inflammation. A few tips for mindful eating include:
- Slow down
- Sit at the table
- Put the fork down between bites
- Don’t eat and watch TV
- Don’t eat straight from the packaging
- Chew more
- Focus on taste
- Close eyes and savor each bite
- Take smaller bites
Patterning
There are several healthy dietary patterns you have likely heard of, including Mediterranean, anti-inflammatory, and low-glycemic. What is important to keep in mind is that all of these have overlapping health generating benefits. More importantly, practitioners should consider individualizing a diet therapy plan to contain elements of these patterns that addresses a patient’s pain and inflammation as well as other health issues, such as elevated blood glucose or obesity. One aspect that should be emphasized is a low glycemic diet, which focuses on foods that are less likely to spike blood sugars (see green column) versus those that are more likely to cause spikes (see red column). This is because low glycemic diets have been shown to reduce inflammation and obesity. This does not mean that foods that are not green cannot be consumed; rather, they should be more carefully planned with healthy fats to minimize glycemic spikes.
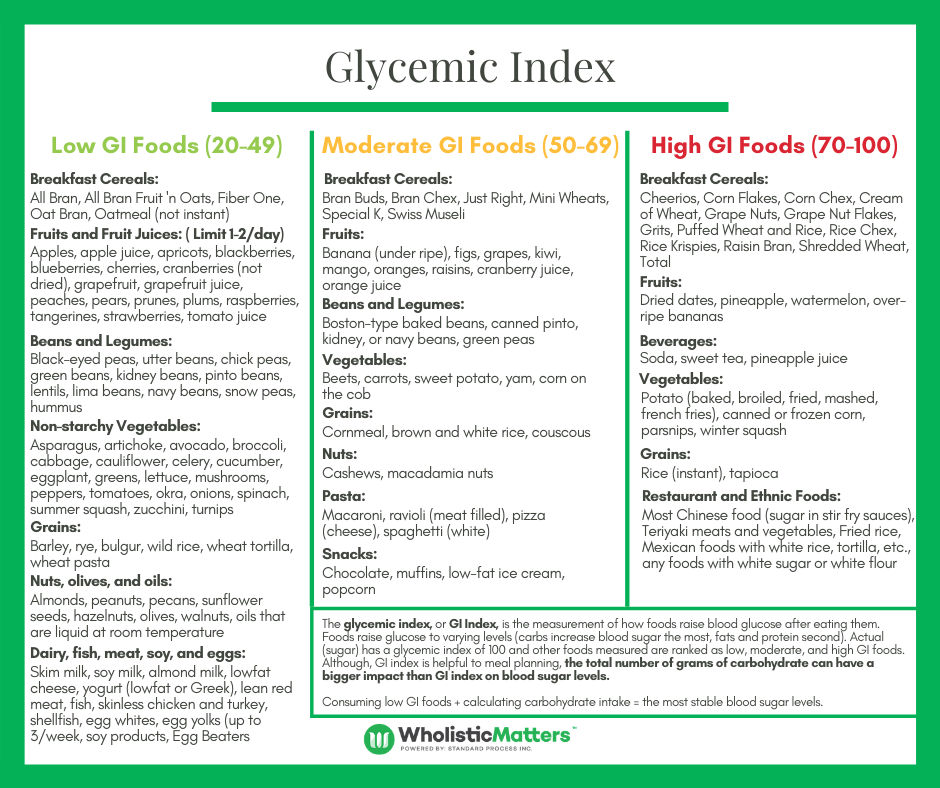
Figure 3: Glycemic Index Foods
Planning
Planning means several things in relation to a patient’s program. First, it means planning the time of their meals with the goal of ideally leaving 12 to 14 hours when they are not eating. This could, for example, mean that they eat a late breakfast at 10 am and dinner by 6 pm with no meals or snacks overnight. This is referred to as Time Restricted Feeding (TRF) or Intermittent Fasting and has been shown to help improve pain and inflammation even when there are no changes in the actual amount of food that is consumed. This is likely related to the concept of helping the body and metabolic machinery rest and focus on other aspects of optimizing the system.
Second, it means planning meals ideally; protein and vegetables are eaten before initial carbohydrate intake. This timing has been shown to reduce insulin and glucose spikes. This is another simple way to reduce glucose spikes and the inflammation that can follow.
The last aspect of planning refers to how a patient will plan meals using recipes and cooking resources provided by the practitioner, as well as how those meals will be combined with medical nutrition therapy (meal replacements) and supplements to help maximize the potential for diet to reduce pain and inflammation. An example of a planning sheet a practitioner could use is seen below.*
Next, practitioners may introduce the patient to the Rs, including:
- Remove
- Reduce
- Replace
- Rest
- Replenish
- Rejuvenate
This important step will help them introduce the key foods that will help reduce inflammation as well as dietary supplements which will support pain relief.
While this program focuses on nutritional approaches, it is important to emphasize the importance of physical activity and how it can help reduce the vicious cycle of pain and inflammation as noted in Figure 4 below.
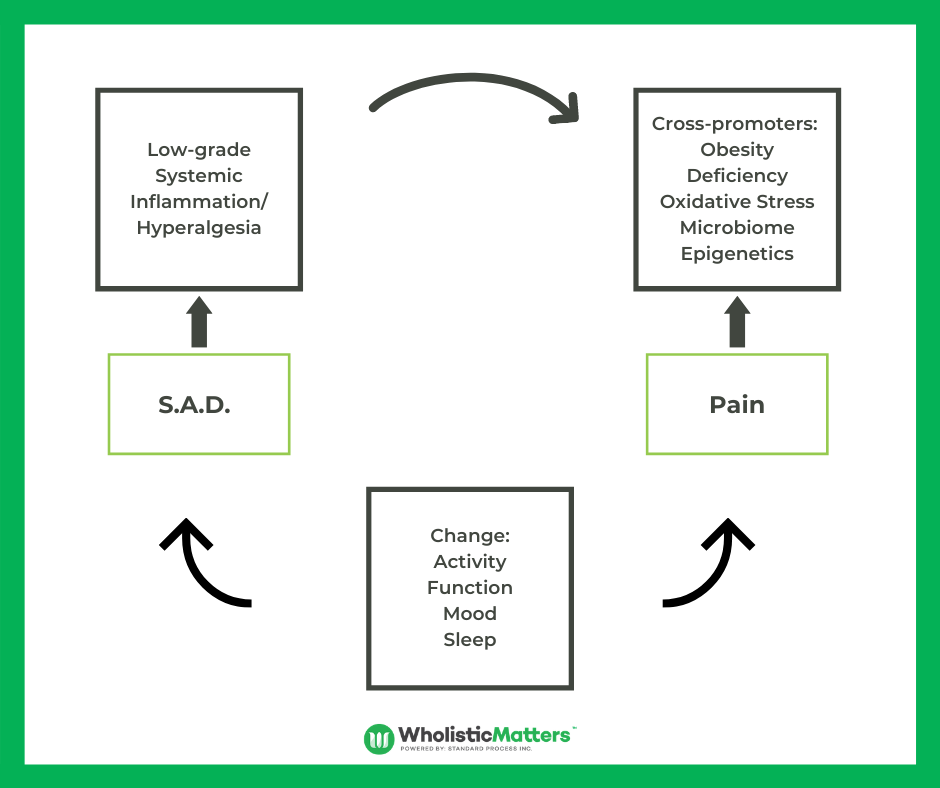
Figure 4: Vicious Cycle of Pain, Lifestyle, Diet and Inflammation
Throughout this process, patients are encouraged to move at their own pace and use their healthcare team to help make optimal choices as well as supporting those choices with physical activity, healthy sleep habits, and stress management to optimize results. Support from the practitioner as well as a specific, individualized diet and supplements are the key in helping the patient stay on track. Practitioners may check in regularly with patients and add the resources and approaches that make the most sense based on their expertise.
After the Ps of Planning, it is important to incorporate the Rs for complete pain relief.
The Rs
- Remove additives and preservatives as well as foods that may create sensitivities from the diet.
- Reduce refined and processed foods.
- Replace with healthier options including anti-inflammatory, low-glycemic, and phytonutrient-rich options.
- Repair and rebalance the gut with foods healthy for the digestive system and supplement choices (pre- and probiotics, digestive enzymes, and herbals).
- Replenish protein and micronutrient stores by focusing on clean dietary stores and bioavailable supplements as directed by a practitioner (magnesium, vitamin D, etc.).
- Reverse and resolve inflammation using healthy fats.
- Rest and rejuvenate by optimizing sleep and making time both for relaxation practices as well as incorporating activity with the guidance of a practitioner.
After reviewing the Ps and Rs of the nutrition plan, a practitioner will be ready to start focusing on supplements.











