Cardiovascular Health: Circulation, Nutrition, and Physical Activity
Cardiovascular Health: Circulation, Nutrition, and Physical Activity
Cardiovascular disease is the leading cause of death in the United States and throughout the world. Consuming a healthy diet, engaging in regular physical activity, and optimizing metabolic health can significantly reduce the risk of developing cardiovascular disease.
What is Cardiovascular Health?
The cardiovascular system includes the heart and blood vessels, which together circulate blood throughout the body. This system runs continuously in the background, often without any noticeable signs, reaching every cell in the body to deliver oxygen and vital nutrients. Cardiovascular health is largely determined by modifiable lifestyle choices, including diet, exercise, and smoking habits; however, other factors can also contribute.1-4 Social factors including stress, job strain, the built environment of a neighborhood as well as the food environment and the availability of healthy foods can also impact cardiovascular health.5
Activity of the Heart Muscle
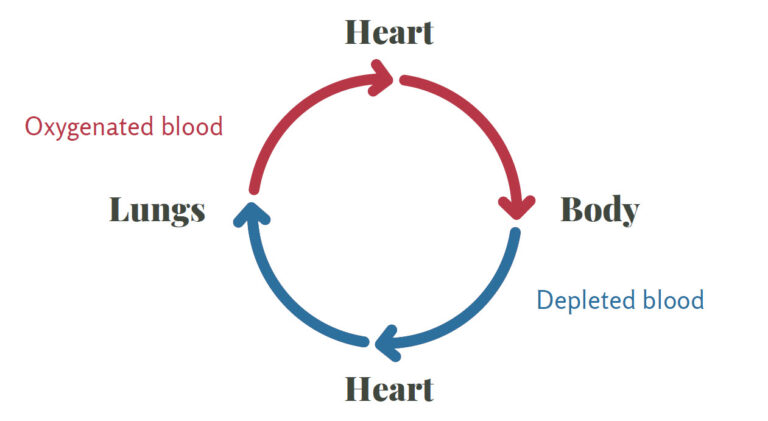
The heart is a muscle that pumps blood throughout the body. It consists of four chambers and four valves that ensure the blood flows only in one direction. Blood travels from every corner of the body to the heart where it enters and is pumped to the lungs to exchange carbon dioxide for oxygen. From there, oxygenated blood returns to the heart, which pumps it out into the body’s circulation system to deliver oxygen and nutrients to organs throughout the body.
Healthy Circulation
The heart works as a central pump, and it needs blood vessels to deliver oxygenated blood to cells throughout the body. Blood vessels, including arteries, veins, and capillaries, permeate every system of the body.
- Arteries primarily carry blood and fluids to organs in the body.
- Veins return depleted blood back to the heart.
- Capillaries are microscopic vessels that transport and exchange nutrients, oxygen, and waste products between the blood and various organs of the body.6
Heart activity can change in response to many stimuli. The brain, kidneys, lungs, skeletal muscle, and skin can all signal increased demand for oxygenated blood as well as release metabolites that regulate cardiovascular action.6 For example, in the first few minutes of physical activity, the heart must adapt to the increased demands of skeletal muscle activity and increase the amount of blood and oxygen it is pumping out. The symptoms of this adaptation can often be felt as an intense beating of the heart and rapid breathing as the heart adjusts. Over time, repeated exercise can improve circulation because of the adaptive changes that occur in the heart. Other events that can trigger changes in the output of the heart include pharmaceutical drugs, electrolytes, hormones, nervous system activity, and adrenal gland secretions.6
Cells of the circulatory system
In addition to blood vessels, several specialized cells improve circulation and oxygen exchange within the cardiovascular system. These cells include cardiomyocytes, endothelial cells, vascular smooth muscle cells, and fibroblasts.
- Cardiomyocytes are the basic cellular unit of the heart.7 They are involved in the excitation and contraction of the heart, allowing it to beat. Cardiomyocytes are electrically and mechanically connected to each other, allowing direct communication and intercellular signaling.7
- Vascular smooth muscle cells are found layered in arteries where they control blood flow and blood pressure by regulating the constriction and dilation of blood vessels.7
- Endothelial cells are regulators of the cardiovascular system.7 They are found in arteries and capillaries as well as the heart where they communicate, serve a structural role, and regulate function of other cells in the heart.7
- Fibroblasts in the heart and blood vessels respond to stimuli, secreting signaling molecules including growth factors and cytokines that affect other cells in the heart.7
Other important cell types include neuronal cells, which control the structure and function of the heart and blood vessels, macrophages that repair blood vessels after an injury and defend the body from pathogens as part of the immune system, and pericytes that communicate between cells in the heart, stabilize blood vessels, and regulate endothelial cell function.7
Common Heart Diseases for Americans
The term “cardiovascular disease” is used broadly to describe conditions ranging from hypertension to vein diseases.4 Typically, it refers to one of four pathologies:8
- Coronary artery disease (or coronary heart disease): the most common heart disease; occurs when the coronary arteries struggle to supply the heart with sufficient blood, oxygen, and nutrients
- Cerebrovascular diseases: conditions that affect blood flow and/or blood vessels in the brain
- Peripheral artery disease: a condition marked by the narrowing or blockage of blood vessels that carry blood from the heart
- Aortic atherosclerosis: a specific type of atherosclerosis involving plaque build-up in the aorta, resulting in conditions such as heart attack, stroke, or sudden loss of blood flow to organs of the body
Atherosclerosis
Atherosclerosis is involved in almost every cardiovascular disease and is heavily influenced by lifestyle factors.8 It is a condition in arteries characterized by plaque formation that can potentially cause cardiovascular disease (CVD) due to decreased or lack of blood flow.8 Blood lipids, immune cells, inflammatory mediators, and dysfunctional endothelial cells initiate the formation of a fatty streak, a visible accumulation of fat in the artery wall that is the first sign of atherosclerosis.8 As cholesterol, fat, blood cells, platelets, macrophages, and other bodily substances aggregate, a plaque forms which limits the amount of blood that can flow through the artery. This narrowing of arteries also limits oxygen delivery to tissues in the body. As layers of plaque form, they secrete chemical messengers that recruit even more cells to the site of “injury” which worsens the condition.8
Significantly reduced blood flow can cause issues in the heart and result in noticeable symptoms; complete blockage of an artery can cause a heart attack. If a plaque bursts, it may result in a blood clot which can travel to other parts of the body and block blood flow. Plaque formation may begin as early as childhood and can eventually lead to an acute cardiovascular event.8
Diagnostics
There are several clinical signs that a healthcare practitioner can evaluate to determine if a patient has an elevated risk for CVD.8 Blood lipid and metabolic panels, often ordered as part of an annual health screening, measure common risk factors that contribute to CVD development:
- Low-density lipoprotein (LDL): a lipoprotein that carries cholesterol throughout the body and is commonly referred to as “bad” cholesterol
- High-density lipoprotein (HDL): a lipoprotein that absorbs cholesterol in the blood and carries it back to the liver where it can be removed from the body; sometimes called “good” cholesterol
- Triglycerides: the most common type of fat in the body; required by the body in small amounts, but too much can contribute to atherosclerosis
- Total cholesterol: the sum of all the cholesterol measures (LDL, HDL, and a portion of the triglyceride measure)
- Blood glucose: an indicator of diabetes or insulin resistance when elevated in the fasted state, which can contribute to poor cardiovascular health
Prevalence
Cardiovascular diseases are the leading cause of death in the United States and globally, making up approximately one out of every four deaths, which equates to about 600,000 deaths in the United States each year.4,8,9 CVD is also the costliest disease, with a projected annual cost of $368 billion by 2035.8
Risk factors
While there are non-modifiable factors that contribute to CVD risk including age and sex, most are modifiable, up to 90 percent. This means almost anyone can reduce their risk of developing CVD with effort and lifestyle changes.1,8 The major risk factors for CVD are:3
- High LDL cholesterol (hyperlipidemia)
- Smoking
- Hypertension (high blood pressure)
- Diabetes
- Abdominal obesity
- Psychosocial factors
- Insufficient fruit and vegetable consumption
- Excessive consumption of alcohol
- Lack of regular physical activity
If all adults in the U.S. attained optimal cardiovascular health, based on the eight recommendations for CVD prevention according to the American Heart Association (AHA), two million CVD events could be prevented each year.10 Even a partial improvement, moving from low to moderate cardiovascular health, could prevent over one million cardiovascular events.10 One estimate suggests that only seven percent of the U.S. population achieves optimal cardiovascular health.10
While cardiovascular diseases are diverse and, in some cases, very complex, their strong relationship to modifiable lifestyle factors allows anyone to maximize their cardiovascular health through lifestyle decisions. The AHA recommends eight behaviors to decrease the risk of CVD, coinciding with many of the risk factors for CVD. They advise adults to:
- Avoid smoking
- Be physically active
- Eat a heart healthy diet
- Get adequate sleep
- Maintain healthy body weight
- Control cholesterol levels
- Manage blood pressure in healthy range
- Achieve blood glucose levels in healthy range4,8,11
In addition to these eight recommendations, maintaining a diverse gut microbiome may positively affect both blood pressure and CVD risk.2,12
Antioxidant Activity for Cardiovascular Health
Oxidative stress is a major underlying pathway that contributes to the development of atherosclerosis and cardiovascular diseases.4 Reactive oxygen species (ROS) and reactive nitrogen species (RNS) are a normal byproduct of cellular process. However, elevated ROS and RNS can lead to oxidative stress, DNA damage, endothelial dysfunction, and increased oxidized LDL particles, which stick to plaques in the arteries, exacerbating plaque formation.4 ROS also negatively affect blood vessels, promoting hypertension, and can impair normal heart function.13 Chronic elevation of ROS can contribute to inflammation, which contributes to the development of cardiovascular diseases.4,13
Antioxidants in the body convert ROS to more stable, less harmful compounds, helping to lessen or prevent oxidative stress. Several nutrients and bioactive compounds possess antioxidant activity including vitamin C, vitamin E, vitamin A, and plant polyphenols. Within the vitamin A family, carotenoids, including beta-carotene and lycopene, combat oxidative stress and protect against CVD.3 Carotenoids are natural compounds found in fresh fruits and vegetables, often in the red and orange category.3 Consuming naturally occurring dietary sources of carotenoids can protect the heart and reduce the risk of developing CVD.14-16 However, clinical trials investigating whether supplementation with isolated carotenoids can deliver the same benefits have not yet found any benefit.3,17
Best Foods for Cardiovascular Health
Diet is one of the most modifiable and consequential lifestyle factors that can positively or negatively impact cardiovascular health. A heart healthy diet can reduce the risk of CVD, and in some cases reverse heart disease.4 It also plays a role in reducing other risk factors that contribute to CVD including obesity, hypertension, diabetes, and hyperlipidemia.4 Following a healthy dietary pattern rich in essential nutrients and whole foods can have a significant impact on cardiovascular health.
B vitamins
Vegetables like spinach, kale, and sweet potatoes are good for cardiovascular health due to the presence of certain B vitamins involved in protecting the heart. Riboflavin (B2), pyridoxine (B6), folate (B9), and cobalamin (B12) are involved in the synthesis and degradation of the amino acid homocysteine. Elevated plasma homocysteine is associated with various vascular diseases, especially in women.3 Maintaining adequate levels of these B vitamins keeps homocysteine levels in a normal range because if any of are in short supply, it can impair enzyme function, leading to a build-up of homocysteine which negatively affects vascular health.
Clinical studies investigating the role of B vitamin supplementation in managing homocysteine levels have produced positive findings. Supplementation with folic acid and vitamin B12 was effective at lowering homocysteine when used together compared to vitamin B6 alone.18 Additionally, supplementation with folic acid, vitamin B12, and vitamin B6 slowed the progression of atherosclerosis in healthy individuals with elevated homocysteine.19 While B vitamin supplementation may help keep homocysteine levels in a healthy range, clinical trials investigating the relationship to cardiovascular diseases have had mixed results. Because of this, supplementation with B vitamins to prevent CVD is considered safe but not routinely recommended. Instead, a balanced diet rich in fruits and vegetables will provide sufficient B vitamins in addition to many other heart healthy nutrients.
The B vitamin niacin (B3) also supports cardiovascular health. It can inhibit inflammatory genes in vascular cells, reduce oxidative stress, and lower cytokines involved in atherosclerosis, improving overall vascular health.3 A supplement form of niacin, nicotinic acid, can raise HDL, lower triglycerides, and, at high doses, lower LDL cholesterol, improving cardiovascular health.20 Niacin can affect blood glucose levels, so it is important to monitor glucose in individuals with diabetes or metabolic syndrome when high doses of niacin are administered.3
| Nutrient | Heart Healthy Food Sources |
| Riboflavin (B2) | Quinoa |
| Salmon | |
| Yogurt | |
| Niacin (B3) | Chicken |
| Sunflower seeds | |
| Salmon | |
| Pyridoxine (B6) | Chickpeas |
| Salmon | |
| Banana | |
| Folate (B9) | Spinach |
| Black-eyed peas | |
| Asparagus | |
| Cobalamin (B12) | Egg |
| Yogurt | |
| Milk |
Omega-3 fatty acids
Fats play an important role in cardiovascular health, but the type of fat is very important. While saturated and trans fats can negatively affect the heart and blood vessels, polyunsaturated fatty acids (PUFAs) actually protect the heart and cardiovascular system. Saturated and trans fatty acids tend to be pro-inflammatory and detrimental to human health, but PUFAs are anti-inflammatory and protect against atherosclerosis.3 Clinical studies evaluating intake of the essential omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) at more than three grams per day have found that they can improve several CVD risk factors, including blood lipids, blood pressure, platelet aggregation, inflammation, and vascular health.3,4
Mediterranean-style diet
Focusing on always achieving the recommended intake of specific nutrients day after day can quickly become overwhelming and exhausting. Instead, adopting a heart-healthy dietary pattern can achieve beneficial health effects and offer flexibility. The best dietary patterns for heart health are the Mediterranean diet and the DASH (Dietary Approach to Stop Hypertension) diet, which share many similarities.1,2 They are associated with low cardiovascular disease risk, and contain many fruits and vegetables, whole grains, and lean sources of protein.1,4 They are also low in processed foods, added sugars and salt, and unhealthy fats.1,4 In one study, people who adhered to this diet had a 14 to 28 percent lower rate of mortality from CVD than individuals who did not.1 Breaking down the features of the Mediterranean diet helps demonstrate the reasons for its heart healthy effects.
Fruits and vegetables
Fruits and vegetables are relatively low in calories but a rich source of fiber, vitamins, minerals, and healthy compounds found only in plants (phytonutrients). Deep-colored plants contain more phytonutrients and consuming a variety of different colored plants will maximize phytonutrient intake.1 For example, a plain white potato does not contain some of the important phytonutrients found in colorful vegetables like broccoli or kale. All forms of fruits and vegetables – fresh, frozen, and canned – can be incorporated into a heart healthy diet.1
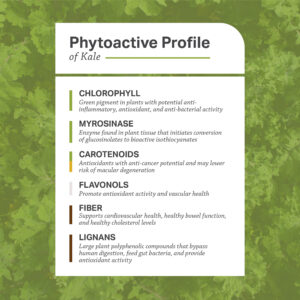
Download the full kale infographic from the Color of Food series.
Whole grains
Whole grains are a good source of fiber, which can lower cholesterol and support a healthy gut microbiome.1,4 Dietary fiber can also improve metabolic healthy by slowing glucose absorption, down-regulate levels of chemicals involved in oxidative stress, and activate a healthy inflammation response by the gut bacteria.4 Choosing whole grains to replace ultra-processed foods provides even more benefits for the heart. Ultra-processed foods are a source of empty calories, lacking fiber and nutrients but full of salt, sweeteners, fats, artificial colors and flavors, and preservatives. These additives enhance shelf-life, texture, and palatability, and can have a highly addictive effect on the body.1,21 In a four-week, randomized study, higher intake of ultra-processed foods led to increased caloric intake and short-term weight gain, a risk factor for CVD.1,22
Lean protein
Protein is found in many different foods, but not all are good for the heart. Sources of lean protein are typically low in saturated fat and minimally processed, such as Greek yogurt, chicken, and salmon. Obtaining protein from fish has an added benefit of adding omega-3 fatty acids to the diet.1 Two to three servings of fish per week has been associated with lower incidence of several types of cardiovascular diseases as well as all-cause mortality.1 Processed meats should be avoided as much as possible due to their relatively low nutritional value and high saturated fat levels.1 They also contain compounds that can be transformed into dangerous metabolites by the gut microbiome, including phosphatidylcholine into trimethylamine N-oxide, as well directly harmful compounds including heterocyclic amines.1
Reduced sodium
A diet high in fruits and vegetables tends to be lower in sodium and higher in potassium, a two-for-one benefit for heart health as sodium tends to increase blood pressure while potassium lowers it.1 The use of spices and whole foods in the Mediterranean diet also naturally reduces sodium levels, which is beneficial for blood vessel health, reducing the risk of hypertension. A Mediterranean-style diet also avoids the most common sources of sodium in the diet- processed foods and packaged foods.1
Other foods and nutrients
The relationship between alcohol and CVD risk remains unclear and controversial; it likely depends on the pattern and amount of alcohol intake, age, and sex.1 Because of the uncertainty and other risks associated with alcohol intake, the AHA does not recommend that individuals begin drinking alcohol solely for their cardiovascular health.1
While research is ongoing, maintaining a heart-healthy dietary pattern can also include adequate intake of nutrients whose roles are not quite clear yet. For example, vitamins K and D may be important in cardiovascular health, although precise mechanisms are not yet known.3,23
Herbs for cardiovascular health
Medicinal herbs have been used both historically and in modern times to address underlying conditions that contribute to poor cardiovascular health. For example, some herbs support components of the cardiovascular system while others promote healthy inflammation. Herbs that counteract inflammation and promote healthy inflammation resolution increase cardiovascular health because inflammation is a major contributor to endothelial dysfunction and plaque formation.24
Culinary spices
Garlic, rosemary, and turmeric are three culinary spices with broad cardio-protective effects.24 Garlic (Allium sativum) can reduce cholesterol and LDL levels, support healthy cardiovascular cell functioning, and combat inflammation and oxidative stress. Together, this makes garlic a powerful herb for protecting against as well as managing atherosclerosis and elevated blood lipids.3,24 Rosemary (Rosemarinus officinalis) and turmeric (Curcuma longa) are also powerful anti-inflammatory herbs, decreasing the expression of pro-inflammatory enzymes and mediators.24
Hawthorn
Hawthorn (Crataegus oxyacantha) is used in Traditional Chinese Medicine to lower cholesterol, which may be due to its ability to upregulate receptors for LDL cholesterol in the liver, resulting in greater uptake which removes it from plasma.3 Hawthorn can also help manage high blood pressure, break down pockets of cholesterol and fat in the body, increase conversion of “bad” cholesterol to “good” cholesterol in the liver, and improve circulation, boosting blood and oxygen supply to the heart.24,25
Gingko
Gingko biloba contains many compounds that mediate inflammation and oxidative stress.3,24 It can also block platelet factors, which can improve atherosclerosis.3,24 In human trials, gingko extract supplementation decreased blood pressure and may yield other benefits related to cardiovascular disease; however, more research is needed as findings have not always been consistent and gingko supplementation can result in side effects.24
Ginseng
Several varieties of ginseng have been studied for their beneficial effects on cardiovascular health. In general, ginseng can improve arterial health, helping to reduce blood pressure and arterial stiffness.3,24 Ginseng is also able to modulate both NF-κB and Nrf2, important cellular regulators of inflammation and oxidative balance.24 In clinical trials, Korean ginseng (Panax ginseng) decreased triglycerides, LDL, and cholesterol levels, increased HDL, normalized inflammatory markers and blood sugar levels, and upregulated antioxidant enzymatic activity.24
Exercise and Cardiovascular Health
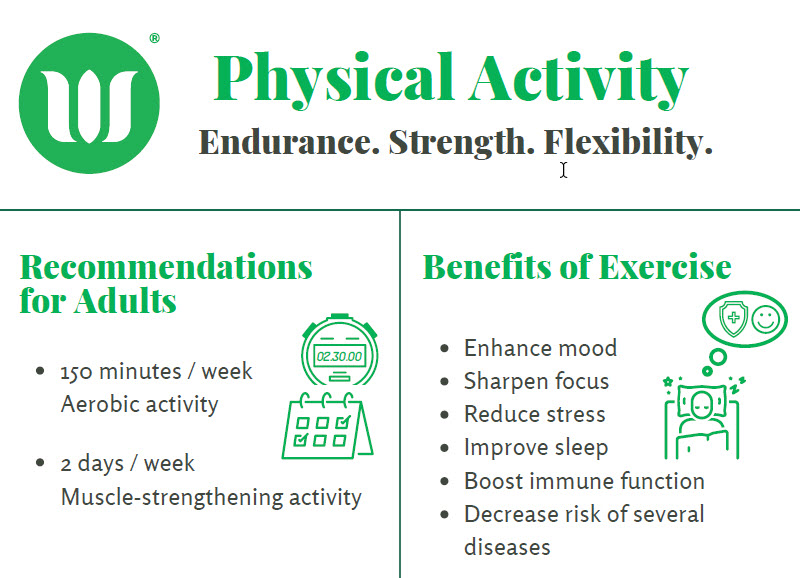
Exercise and cardiovascular health act as a two-way street. Exercising muscles need the cardiovascular system to receive oxygen and nutrients from circulating blood. In turn, exercise improves cardiovascular health and circulation, enabling improved, more efficient delivery in the future. Physical activity is linked to a reduction in mortality from any cause, not just cardiovascular diseases, although it likely protects from mortality by reducing the risk of cardiovascular diseases.9 Even if individuals have other risk factors for CVD, exercise still reduces rates of death in both men and women.9 It is also associated with a healthier inflammatory profile, decreased risk of heart failure, and improved survival for individuals with coronary artery disease up to 30 years after initiation of a workout regimen.9
The benefits of engaging in regular physical activity have significant overlap with risk factors for cardiovascular disease, including hyperlipidemia, hypertension, insulin resistance, and abdominal obesity. Exercise also targets underlying mechanisms and contributing factors including inflammation, sleep, and heart function.2,9,26 Over time, the body adapts to chronic exercise by remodeling the heart, altering mitochondrial biogenesis, and fatty acid oxidation, as well as pumping blood more efficiently.9 Together, these greatly increase cardiovascular system health.9
| CVD Risk Factor or Contributing Pathway | Benefit of Exercise |
| Elevated blood lipids | Decreased LDL and increase HDL |
| Dysregulated glucose metabolism and insulin resistance | Enhanced insulin sensitivity and uptake of glucose into cells |
| High blood pressure | Decreased blood pressure |
| Overweight/obesity; abdominal adiposity | Increased caloric burn, potentially increasing weight loss |
| Atherosclerosis | Promotes regression of atherosclerotic lesions |
| Mechanical ability of heart and blood vessels | Enhances remodeling of heart and artery walls |
Current guidelines call for at least 150 minutes of moderate-intensity exercise per week.1 Moderate intensity physical activity raises the heart rate but still allows participants to carry out a conversation. More intense exercise can provide even more benefits, but is not necessary to begin seeing positive changes in metabolic and cardiovascular health.9 For example, going for an evening walk with the dog can increase heart health (for the dog too!).
Health Benefits of Physical Activity
3 Types of Physical Activity
Physical activity is recommended for nearly all Americans, from preschool-aged children through adulthood. Engaging in a range of activities can lead to significant positive changes in the body.
How to Improve Cardiovascular Health
Both major and minor changes in dietary habits and health behaviors can have a significant impact on cardiovascular health, circulation, and metabolic health. Refraining from smoking is one of the biggest choices that can significantly improve cardiovascular health, followed by adopting a heart-healthy diet, similar to a Mediterranean-style diet full of fruits, vegetables, lean protein, omega-3 fatty acids, and fiber. Other avenues for support include consuming heart health-promoting herbs and obtaining adequate physical exercise. Together, these choices can greatly reduce the risk of developing cardiovascular disease.
WholisticMatters is powered by Standard Process, a nutritional supplement company family-owned and operated for over 90 years. Standard Process offers many nutritional solutions.