Prebiotics, Whole Food Fiber and Herbs for Optimal Digestive Health
Managing Digestive Health with Prebiotics and Probiotics
Digestive complaints are one of the primary driving factors that encourage individuals to seek out alternative health care options, including nutrition and herbs. Many of these digestive complaints can trace their roots to imbalances in the microbiome – the complex ecosystem of bacteria, fungi and viruses- that exist in the human gut.1,2 Even aspects of health and wellness outside of digestive function have been linked to the integrity of this rich microbial network, including mental health and immune function.
Eating fermented foods like yogurt, kimchi and sauerkraut, as well as supplementing with probiotics, can help to encourage the populations of beneficial bacteria in the gut. Just as important as consuming beneficial bacteria, however, is consuming the fuel those bacteria need in order to thrive: prebiotics. Prebiotics are a type of complex carbohydrate, such as inulin and certain oligosaccharides, that the human body cannot digest but that function as fuel for the beneficial bacteria in the gut.3
These prebiotics are arguably more foundational for a healthy microbiome than probiotics because they act as a ‘fertilizer’ for established beneficial gut bacteria, promoting a diverse and resilient ecosystem. While probiotics introduce new bacteria, they won’t thrive or create lasting changes without the prebiotic fiber to feed them. Learning how to nourish and support the microbiome offers an incredible opportunity to expand the narrative around therapeutic options for improving well-being on numerous levels.
Prebiotic 2’FL: Made for the Microbiome
2′-Fucosyllactose (2’-FL) is a human milk oligosaccharide (HMO) that functions as a prebiotic in the human digestive system.7 2’-FL is the most abundant HMO found in breast milk, and the first prebiotic compounds that a breastfed newborn will encounter to feed their developing microbiome.

HMOs avoid metabolism by digestive enzymes until they reach the lower gastrointestinal (GI) tract, which allows beneficial microorganisms like Bifidobacteria to then break them down through fermentation.8,9 In addition to acting as an important component of a newborn’s microbiome and healthy GI tract, 2’-FL also works as a targeted prebiotic for adults due to its unique tie to Bifidobacteria. For adults, 2’-FL supports short-term feeding of beneficial Bifidobacteria in times of GI stress and for individuals deficient in Bifidobacteria populations looking to increase microbiome diversity.10 One study showed that 5 g of 2’FL daily for just two weeks modified the microbiome in favor of these beneficial species.7
Like 2’FL, certain foods have been recognized for their beneficial impact on microbial diversity and function. Okra, for example, is rich in a soothing, gel-like mucilage that functions as a prebiotic food source for gut bacteria and soothes irritation and inflammation in the lining of the gut that may contribute to dysbiosis. Okra consumption has been shown to increase beneficial bacteria like Lactobacillus and Akkermansia, decrease potentially harmful species like Proteobacteria, and promote the production of Short Chain Fatty Acids (SCFAs), compounds that are crucial for digestive and systemic health.8,9

Similarly, beets are rich in prebiotic fiber, such as pectin and pectic-oligosaccharides, that are able to positively modulate gut microbiota composition, as well as encourage the growth and function of probiotic species.10 Beet betalains and phenolics increase the production of SCFAs by gut microbiota and possess significant antioxidant, anti-inflammatory and anti-carcinogenic properties that have been shown to improve overall gastrointestinal health.10
Probiotic Highlight: Bifidobacteria
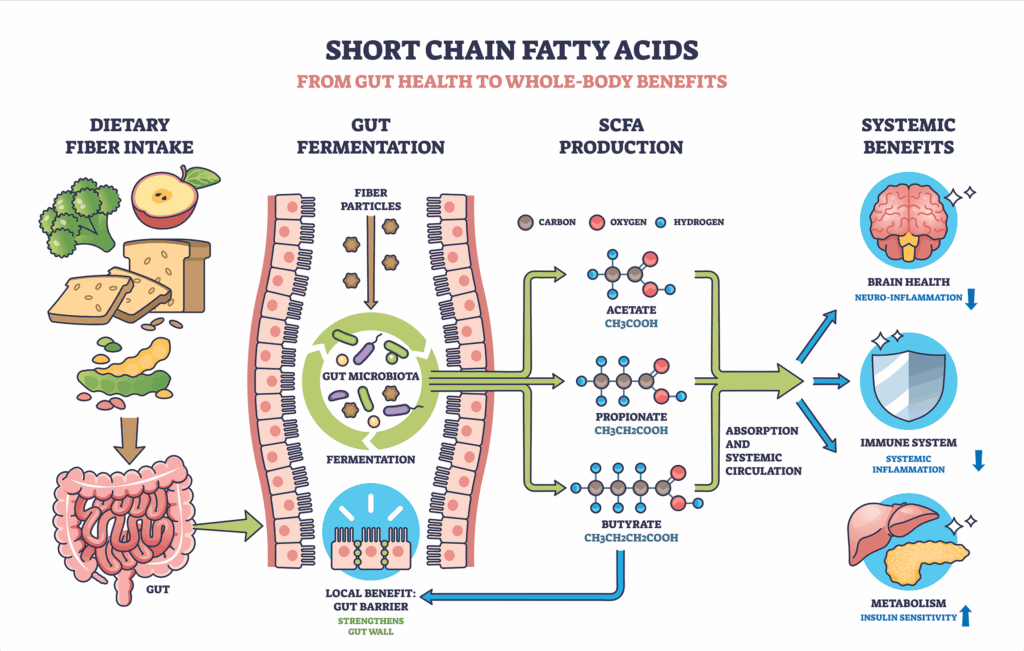
While diversity of species in the microbiome is essential for the ecosystem’s health and vitality, the Bifidobacteria genus stands out as a key therapeutic target for improving digestive health, as well as mitigating inflammation and improving mental health. One of the most valuable functions of Bifidobacteria is their role in Short Chain Fatty Acids (SCFAs) production. When Bifidobacteria species digest prebiotic fiber, such as 2’FL, they produce SCFAs, primarily acetate, propionate, and butyrate, which are key signaling molecules and energy sources for the colon.
The Functions of SCFAs:
- Intestinal integrity: the main energy source for the colon, butyrate supports mucosal integrity and repair, maintaining tight junctions within the gut and reducing intestinal permeability.11
- Regulation of gut pH: SCFAs lower the pH of the colon, which inhibits the growth of pathogenic bacteria and promotes the survival of beneficial bacterial strains.12
- Inflammation & immune modulation: SCFAs modulate immune cell activity in the gut, including pro-inflammatory cytokines (like TNF-α and IL-6) and promote anti-inflammatory T-regulatory cells.13 SCFAs communicate with immune cells throughout the body, helping to maintain immune tolerance and contributing to lower risk of autoimmune and chronic inflammatory diseases.14
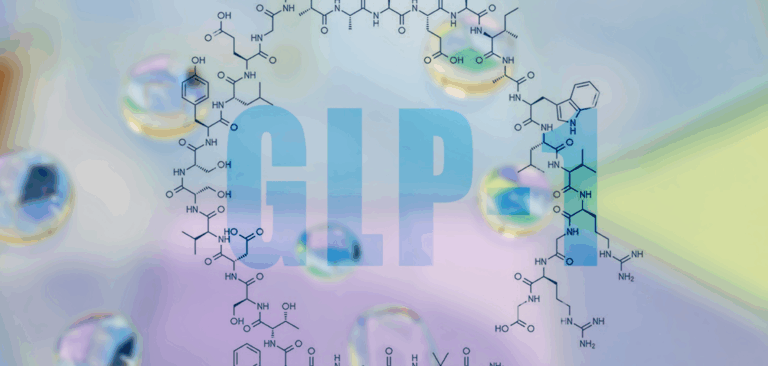
- Metabolic regulation: propionate is directly involved in the process of gluconeogenesis in the liver, contributing to blood sugar balance and insulin sensitivity.15 SCFAs also stimulate the release of satiety hormones such as GLP-1 and PYY, improving insulin sensitivity.16
- Nervous system stability: Through the gut-brain axis, SCFAs may influence neurotransmitter production and neuroinflammation. Butyrate, in particular, acts as a histone deacetylase (HDAC) inhibitor, affecting gene expression related to brain health and mood regulation.17,18
The wide ranging effects of SCFA production through key Bifidobacteria species highlight the therapeutic potential for encouraging a stronger gut Bifidobacteria population. Conditions including Functional Gastrointestinal Diseases like IBS, obesity and Metabolic Syndrome, mood disorders and even autoimmune disease may benefit from both seeding and feeding Bifidobacteria.
HMOs Support the Gut Barrier in the Lower GI
Healthy gut function relies on a proper GI barrier between the body and the interior space that makes up the digestive tract, called the lumen. The GI barrier is made up of many layers:
- Luminal mucosal barrier
- Microbial inhabitants lining cells in the lumen
- Layer of mucus produced by goblet cells
- Chemical barrier
- Physical barrier of intestinal epithelial cells held together by tight junctions
- Immunological barrier

Stress, microbial invaders, antibiotic use, and development of chronic conditions can disrupt the intestinal lining. HMOs like 2’-FL stimulate the development and maintenance of a well-functioning GI barrier, both during development and in cases of GI inflammation.19-21
Through the gut-brain axis, SCFAs may influence neurotransmitter production and neuroinflammation. Butyrate, in particular, acts as a histone deacetylase (HDAC) inhibitor, affecting gene expression related to brain health and mood regulation.
Whole Foods and Herbs to Support the Gut Barrier
Herbs and foods also have a key role in strengthening this mucosal barrier. While prebiotics like 2’FL function as food or fertilizer for beneficial bacteria, key herbs and foods are able to tend the ‘soil’ in which those probiotic species thrive through their impacts on mucous membrane health. Medicinal plants have a long history of use in supporting digestive function: bitter herbs such as gentian and dandelion root for stimulating digestive secretions and improving peristalsis, carminative herbs including ginger and chamomile for relieving bloating and discomfort, and digestive tonic herbs such as meadowsweet and licorice for improving the integrity of the gut mucosa.
The gut mucosal layer and microbiome are connected through a symbiotic, reciprocal relationship where the mucosal layer acts a habitat for microbes, while a healthy microbiome helps to regulate the mucosa’s structure and function. Digestive tonic herbs can help facilitate this symbiotic relationship by strengthening the integrity of the mucus layer and encouraging the repair of the digestive lining, creating a healthier habitat for the beneficial microbes. One lesser-known digestive tonic is Collinsonia canadensis, also known as stoneroot or heal-all, alluding to both the sheer density of the root and the multitude of applications used by traditional healers.

Collinsonia has a rich history of use by indigenous North American peoples and early Eclectic physicians for improving the functioning of the gut, respiratory system and genitourinary tract- with the key commonality in these systems being the root’s affinity for improving mucosal health and tonifying vasculature. This astringent or tonic effect of the root made it a key remedy in the treatment of hemorrhoids, varicose veins and even laryngitis.22
Specific to the gut, Collinsonia was used as a ‘stimulant and tonic in cases of atonic dyspepsia, and in chronic disease with feeble digestion’22 – conditions that negative impact the health and function of the microbiome. By strengthening the integrity of the soil- the mucosal layer- in which beneficial microbes thrive, Collinsonia serves as an active partner to prebiotics like 2’FL in maintaining the health of the microbiome.
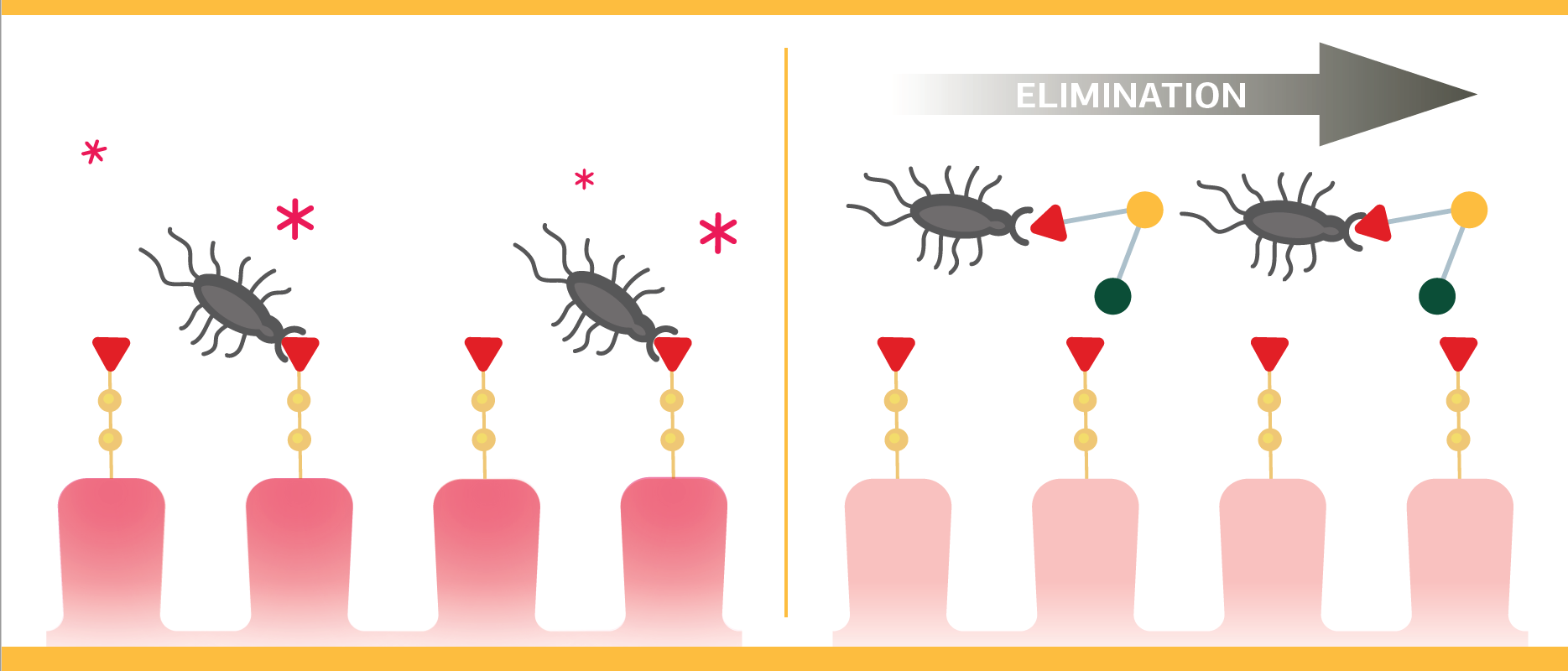
Gut Immunity: 2’-FL as a “Binding Decoy”
Beyond its role as a nourishing ‘fertilizer’ for the microbiome, 2’FL functions as a binding decoy in the gut by mimicking the structures on intestinal epithelial cells that many pathogens use to attach and initiate infection- a key role in the prebiotic’s ability to support not just mucosal health but systemic immunity as well. HMO’s like 2’-FL can competitively bind to bacterial lectins or viral adhesion proteins, effectively blocking these pathogens—such as Campylobacter jejuni, E. coli, and certain noroviruses—from adhering to the gut lining.5,23,24 Additionally, this mechanism helps maintain mucosal integrity, reduces inflammation, and promotes immune tolerance in the developing gut, making it especially important for infants but also potentially beneficial in adult gut health formulations.
Clinical Takeaways

Improving the microbiome isn’t just about probiotic intake—it’s about creating the right environment for those microbes to flourish. Prebiotics like 2’-FL, along with prebiotic-rich foods such as okra and beets, provide the essential “fuel” that sustains beneficial bacteria like Bifidobacteria and promotes the production of short-chain fatty acids crucial for gut integrity, immune balance, and even mood regulation. Pairing these targeted prebiotics with herbs that strengthen the mucosal barrier—such as Collinsonia—creates a comprehensive strategy for restoring gut resilience from the inside out.
The microbiome is a rich, diverse ecosystem that needs to be cultivated and nourished, particularly in the face of modern challenges to microbiome health like the Standard American Diet and environmental toxins. Tools for microbiome management like prebiotics and herbs are a unique tool for allowing clinicians and their patients to move beyond symptom management toward true digestive and systemic wellness.
Did you know WholisticMatters is powered by Standard Process? Learn more about Standard Process’ whole food-based nutrition philosophy.
- Xiong RG, Li J, Cheng J, et al. The Role of Gut Microbiota in Anxiety, Depression, and Other Mental Disorders as Well as the Protective Effects of Dietary Components. Nutrients. Jul 23 2023;15(14)doi:10.3390/nu15143258
- Wiertsema SP, van Bergenhenegouwen J, Garssen J, Knippels LMJ. The Interplay between the Gut Microbiome and the Immune System in the Context of Infectious Diseases throughout Life and the Role of Nutrition in Optimizing Treatment Strategies. Nutrients. Mar 9 2021;13(3)doi:10.3390/nu13030886
- Carlson JL, Erickson JM, Lloyd BB, Slavin JL. Health Effects and Sources of Prebiotic Dietary Fiber. Curr Dev Nutr. Mar 2018;2(3):nzy005. doi:10.1093/cdn/nzy005
- Medina DA, Pinto F, Ovalle A, Thomson P, Garrido D. Prebiotics Mediate Microbial Interactions in a Consortium of the Infant Gut Microbiome. Int J Mol Sci. Oct 4 2017;18(10)doi:10.3390/ijms18102095
- Bode L. Human milk oligosaccharides: every baby needs a sugar mama. Glycobiology. Sep 2012;22(9):1147-62. doi:10.1093/glycob/cws074
- Hirvonen J, Salli K, Putaala H, Tiihonen K, Maukonen J, Ouwehand A. Selective Utilization of Human Milk Oligosaccharides 2’-FL and 3-FL by Probiotic Bacteria Resulting in Different Metabolite Production by These Bacteria (P20-012-19). Current Developments in Nutrition. 2019/06/01/ 2019;3:nzz040.P20-012-19. doi:https://doi.org/10.1093/cdn/nzz040.P20-012-19
- Elison E, Vigsnaes LK, Rindom Krogsgaard L, et al. Oral supplementation of healthy adults with 2′-O-fucosyllactose and lacto-N-neotetraose is well tolerated and shifts the intestinal microbiota. Br J Nutr. Oct 2016;116(8):1356-1368. doi:10.1017/s0007114516003354
- Wu J, Cao M, Hu M, et al. Intervention Effects of Okra Extract on Brain-Gut Peptides and Intestinal Microorganisms in Sleep Deprivation Rats. Evid Based Complement Alternat Med. 2022;2022:9855411. doi:10.1155/2022/9855411
- Zhang J, Zhao Y, Ren D, Yang X. Effect of okra fruit powder supplementation on metabolic syndrome and gut microbiota diversity in high fat diet-induced obese mice. Food Research International. 2020/04/01/ 2020;130:108929. doi:https://doi.org/10.1016/j.foodres.2019.108929
- de Oliveira SPA, do Nascimento HMA, Sampaio KB, de Souza EL. A review on bioactive compounds of beet (Beta vulgaris L. subsp. vulgaris) with special emphasis on their beneficial effects on gut microbiota and gastrointestinal health. Crit Rev Food Sci Nutr. 2021;61(12):2022-2033. doi:10.1080/10408398.2020.1768510
- Scharf MW, Forsgård RA, Prado SBR, et al. Acute effects of butyrate on intestinal permeability in patients with irritable bowel syndrome assessed by a novel colonoscopy research model. Gut Microbes. 2025/12/31 2025;17(1):2545414. doi:10.1080/19490976.2025.2545414
- Nogal A, Valdes AM, Menni C. The role of short-chain fatty acids in the interplay between gut microbiota and diet in cardio-metabolic health. Gut Microbes. Jan-Dec 2021;13(1):1-24. doi:10.1080/19490976.2021.1897212
- Vinolo MA, Rodrigues HG, Nachbar RT, Curi R. Regulation of inflammation by short chain fatty acids. Nutrients. Oct 2011;3(10):858-76. doi:10.3390/nu3100858
- Liu X-f, Shao J-h, Liao Y-T, et al. Regulation of short-chain fatty acids in the immune system. Frontiers in immunology. 2023;14:1186892.
- Zhan K, Yang TY, Chen Y, Jiang MC, Zhao GQ. Propionate enhances the expression of key genes involved in the gluconeogenic pathway in bovine intestinal epithelial cells. Journal of dairy science. 2020;103(6):5514-5524.
- Tang R, Li L. Modulation of Short-Chain Fatty Acids as Potential Therapy Method for Type 2 Diabetes Mellitus. Can J Infect Dis Med Microbiol. 2021;2021:6632266. doi:10.1155/2021/6632266
- Bourassa MW, Alim I, Bultman SJ, Ratan RR. Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health? Neurosci Lett. Jun 20 2016;625:56-63. doi:10.1016/j.neulet.2016.02.009
- Silva YP, Bernardi A, Frozza RL. The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front Endocrinol (Lausanne). 2020;11:25. doi:10.3389/fendo.2020.00025
- Li A-l, Ni W-w, Li Y, et al. Effect of 2′-fucosyllactose supplementation on intestinal flora in mice with intestinal inflammatory diseases. International Dairy Journal. 2020/11/01/ 2020;110:104797. doi:https://doi.org/10.1016/j.idairyj.2020.104797
- Holscher HD, Davis SR, Tappenden KA. Human Milk Oligosaccharides Influence Maturation of Human Intestinal Caco-2Bbe and HT-29 Cell Lines12. The Journal of Nutrition. 2014/05/01/ 2014;144(5):586-591. doi:https://doi.org/10.3945/jn.113.189704
- Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392. doi:10.3389/fncel.2015.00392
- King J. King’s American dispensatory. vol 2. Ohio Valley Company; 1909.
- El-Hawiet A, Kitova EN, Klassen JS. Recognition of human milk oligosaccharides by bacterial exotoxins. Glycobiology. 2015;25(8):845-854.
- Newburg DS. Do the Binding Properties of Oligosaccharides in Milk Protect Human Infants from Gastrointestinal Bacteria?12. The Journal of Nutrition. 1997/05/01/ 1997;127(5):980S-984S. doi:https://doi.org/10.1093/jn/127.5.980S