Clinical Considerations for Athlete Blood Glucose Levels
Understanding Blood Glucose Levels
Glucose is the primary fuel for the body. It provides energy to organs which allows cells to function properly. Carbohydrate-containing foods are a major source of glucose in the blood, although the breakdown of stored glycogen molecules also contributes under certain conditions.
The hormones insulin and glucagon work in tandem to keep blood glucose concentration in a specific range. Insulin decreases blood glucose by signaling cells to import glucose while glucagon helps raise blood glucose levels by signaling glycogen breakdown. Hyperglycemia, or high blood sugar, can damage blood vessels and contribute to the development of obesity, metabolic syndrome, and cardiovascular disease. On the other hand, low blood sugar, hypoglycemia, can result in serious complications including coma or death.1
Blood Glucose Measurements
Blood glucose measurements can be taken in either the fasted or fed state. Non-fasting blood glucose will typically be higher than fasting levels due to the breakdown of carbohydrates from a recently consumed meal and levels below 140 mg/dL are considered in a healthy range. Fasting blood glucose gives the most accurate view of the state of blood glucose metabolism in the body and is also used to diagnose type 2 diabetes and pre-diabetes.
| Fasting Blood Glucose Concentration | |
| < 99 mg/dL | Normal |
| 100-125 mg/dL | Pre-diabetes |
| >126 mg/dL | Diabetes |
Diet is the biggest determinant of non-fasting blood glucose levels. Easily digestible carbohydrates cause a sharp, steep rise in blood glucose while indigestible carbohydrates produce a more blunted curve. Proteins and fats can impact blood glucose levels, primarily by slowing digestion resulting in a less intense spike after a meal. Protein may contribute to overall glucose metabolism although its effect is usually not a major determinant of overall blood glucose concentration. Other factors that impact blood glucose include:
- Medications
- Underlying health conditions
- Stress
- Physical activity
Importance of Blood Glucose Levels in Athletic Performance
Physical activity significantly increases the energy demands on the body, especially in skeletal muscle which relies on glucose for proper functioning during a variety of exercises. Without sufficient glucose, cellular function can become impaired, leading to decreased athletic performance, faster time to exhaustion, and delayed recovery.2
Low blood sugar, also called hypoglycemia, can result in feelings of fatigue, nausea, headache, and paleness. However, high blood sugar, or hyperglycemia, can negatively impact athletic performance by impairing normal energy production pathways in the body, including in muscle, and may also promote muscle atrophy.3 Therefore, consuming proper amounts of macronutrients, especially carbohydrates, before, during, and after physical activity can have a profound positive impact on exercise response, athletic performance, muscle growth, and aerobic fitness by maintaining blood glucose levels in the desired range.4
Normal Range of Blood Glucose Levels for Athletes
Blood glucose homeostasis is a high priority for the body. Blood glucose concentrations are generally kept between approximately 70-140 mg/dL (4-8mmol/L) and are regulated by hormones as well as muscle contraction.5
Athletes should aim for blood glucose to fall between 126-180 mg/dL (7-10 mmol/L) before beginning exercise.6 Below this level, the body may not have enough blood glucose supply to safely exercise and concentrations far above this range (<270 mg/dL or 15 mmol/L) can result in a potentially dangerous condition called ketoacidosis in certain populations. To maintain blood glucose concentration in a relatively narrow range, athletes may need to replenish glucose levels during intense or prolonged exercise.7
If blood glucose levels are just below the ideal range, ten grams of easily digestible carbohydrates can help increase blood glucose concentration while 15 to 30 grams of carbohydrates may be required if blood glucose levels are significantly lower before exercise. Consuming easily digestible carbohydrates during intense or prolonged exercise will allow for rapid digestion, absorption, and appearance of glucose in circulation while also avoiding unwanted gastrointestinal issues that can arise due to high fiber consumption.
If blood glucose is over 180 mg/dL (10 mmol/L), it is still safe to exercise but caution should be taken as some strength training or high intensity interval training regimens may increase blood glucose. Finally, if blood glucose is over 270 mg/dL (15 mmol/L), it may be dangerous to exercise until levels decrease to a healthy range.
Impact of Physical Activity on Blood Sugar Levels
Skeletal muscle is an important player in glucose metabolism, taking up glucose after a meal which helps lower blood glucose levels and serving as a primary glycogen storage location.4,8 During exercise, glucose uptake in muscle is increased up to 50-fold compared to uptake at rest and remains elevated for a period of time after exercise.5,8 The liver also increases glucose production during exercise to keep blood glucose levels stable.8 For endurance events longer than two hours, catecholamine release also influences blood glucose levels by increasing glucose production.8
At relatively low intensity aerobic activity, as measured by VO2max or the maximum amount of oxygen the body absorbs and can utilize during a workout, about 10-15 percent of energy production comes from carbohydrates. As intensity increases, the body’s reliance on glucose increases as it is a quick source of energy compared to the oxidation of fats.4 Most sports and exercises amount to an effort between 60 to 70% VO2max, where muscle glycogen and blood glucose are the primary source of energy.4
Because physical activity can deplete blood glucose and glycogen stores, and loss of glycogen reserves is one of the determinants of muscle fatigue, replenishing with carbohydrates before, during, and after exercise can help prolong exercise, increase measures of athletic performance, and re-establish glycogen reserves.4
The Positive Effects of Physical Activity
In general, physical activity has an overwhelmingly beneficial effect on blood glucose levels. In the short-term, physical activity benefits blood glucose metabolism through increased uptake of glucose into muscles, helping decrease blood glucose levels and increase insulin sensitivity.9 Longer term benefits arise from organ crosstalk among skeletal muscle, liver, pancreas, and adipose tissue which favorably regulate blood glucose levels, blood lipids, and blood pressure.9
Physical activity can also impact long-term measures of blood glucose homeostasis, including HbA1c, which is affected by both exercise duration and intensity.8 While one round of exercise can result in beneficial regulation of blood glucose levels, regular exercise results in sustained improvements in both insulin sensitivity and glucose disposal in skeletal muscle.9
Role of Aerobic Exercises in Regulating Blood Glucose Levels
Aerobic exercise is any activity that increases heart rate and oxygen utilization. It requires the activity of large muscle groups and is typically rhythmic and repetitive. Aerobic exercise includes activities such as swimming, dancing, or running. It provides many benefits for blood glucose levels as well as overall health.
In fact, it is routinely recommended for individuals with diabetes and can help:
- Normalize glucose levels, blood pressure, and lipid dysregulation.
- Improve glycemic control, insulin sensitivity, oxidative capacity, and other metabolic parameters.
- Aid in weight loss.8,9
How Aerobic Exercise Lowers Blood Glucose Levels
A unique characteristic of aerobic exercise is that it helps reduce blood glucose levels through insulin-independent mechanisms. Under standard, insulin-dependent pathways, the body signals the pancreas to release insulin when it detects an increase in blood glucose. Insulin then initiates a signaling cascade in cells to move glucose transporters to the surface. There they can import glucose, taking it out of the blood and, in turn, lowering blood glucose levels.
Aerobic exercise has the same effect but is not dependent on insulin. Instead, exercise results in the recruitment GLUT4, a glucose transporter, to the cell surface, helping facilitate the entry of glucose into the cell which lowers blood glucose levels.8 Because this pathway is insulin-independent, it can help increase insulin sensitivity as less insulin is needed to achieve glucose homeostasis, thus preventing desensitization of cells and tissues to insulin.9
Aerobic exercise can also activate AMPK, a fuel-sensing enzyme in skeletal muscle that helps regulate glucose transport, lipid and protein synthesis, and nutrient metabolism.10 AMPK can stay activated even after exercise concludes, exerting beneficial effects on mitochondrial function and metabolism.9
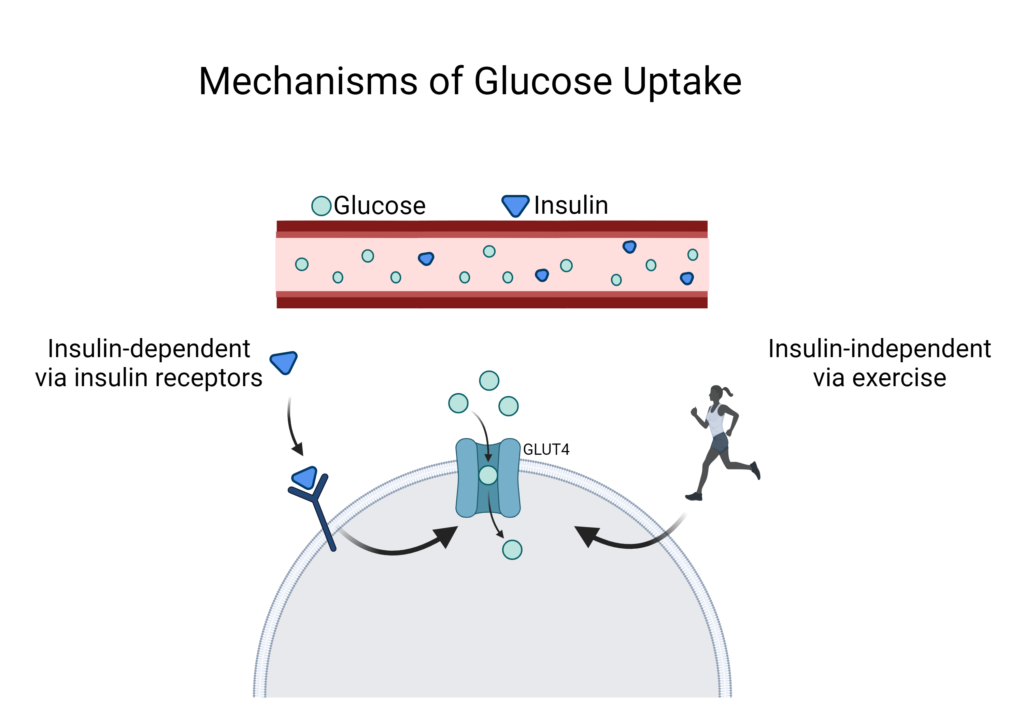
Created with BioRender.com
While one bout of aerobic exercise can provide benefits to the body, the CDC and American Diabetes Association (ADA) recommend 150 minutes of moderate intensity each week. Moderate activity includes any activity that allows participants to talk, but not sing.
Intense physical activity, on the other hand, makes it so the participants can no longer comfortably talk while carrying out the activity. Aim for five to six days of activity per week, with no more than 48 hours in between exercise sessions. Combining aerobic exercise with resistance training may also be more effective in keeping blood glucose levels in a healthy range.9
Effect of High-Intensity Interval Training on Blood Glucose Levels
High-intensity interval training (HIIT) is considered an “all-out” effort, often with an intensity over 90% VO2max.8 During HIIT workouts, glucose is the primary energy source, but if aerobic capacity is exceeded, the body will produce lactate via anaerobic metabolic pathways.8
Catecholamines also play an important role during HIIT as they tend to significantly increase, leading to a seven- or eight-fold increase in glucose production.8,11 While this sounds beneficial, the increase in glucose utilization is less than the production, increasing only about three to four-fold which can result in an increase in blood glucose levels.8,9,11
This increase in blood glucose levels during HIIT continues immediately after the exhaustion point and can persist for up to an hour after the exercise has finished as muscle glucose uptake capabilities are sharpy lowered at the end of a workout.5,8 Additionally, as a part of the body’s natural response to high blood glucose, it releases more insulin, potentially resulting in a period of transient insulin resistance.8,12 Despite this transient state, many studies confirm that HIIT increases insulin sensitivity for several weeks after a training regimen.8
Consumption of simple carbohydrates during HIIT, similar to endurance events, can help stabilize blood sugar and normalize cellular signaling cues to prevent hyperglycemia. For all athletes, HIIT requires special consideration to maintain sufficient blood glucose levels and proper hydration. This will help enable optimal athletic performance and recovery.
Continuous Glucose Monitoring for Athletes
Continuous glucose monitoring (CGM) offers near-real time data on blood glucose levels. It is commonly used in individuals with diabetes to help manage blood glucose levels without painful finger pricks, but potential applications have spread to the athletic world, with the goal of optimizing nutrition and training program for peak performance.
Continuous glucose monitoring systems work by measuring interstitial glucose levels in real time.7 The interstitial layer falls between the skin and blood vessel and reflects blood glucose concentrations but with a 5–10-minute delay.7
The sensor of a CGM system is inserted into subcutaneous tissue, such as the abdominal wall, upper buttocks or back of the upper arm.7 These sensors typically last three to 14 days, but that can depend on the type of sensor as well as water and sweat exposure, heat, and direct physical contact.7
Many CGM systems use an electrode soaked in glucose oxidase, which catalyzes a reaction with glucose and produces an electrical current that corresponds to the concentration of glucose.7 The device sends this information to a receiver, commonly a smartphone app, which allows the user to see near-real time glucose fluctuations, however there is a slight delay of 5-10 minutes in the interstitial glucose concentration.7 Many CGM apps allow users to manually record daily carbohydrate intake and exercise, but interpretation of data can still be complicated. Additionally, some CGM systems require user-facilitated calibration, often through blood glucose testing via glucometer, while others are calibrated in the factory laboratory during manufacturing.7
MODD and MAGE Considerations
In addition to glucose concentrations, athletes may find other measures of glycemic variability useful including the mean of daily differences (MODD) and mean amplitude of glucose excursion (MAGE).7 MODD is calculated as the mean of differences between glucose values at the same time but on consecutive days, allowing it to give insight into differences from day to day.7 A higher MODD represents larger day-to-day variations in whole-body glycemia and is associated with negative outcomes.7 MAGE quantifies major fluctuations in glucose within a 24-hour period and is a more widely used CGM measure of intra-day differences in blood glucose concentrations.7
Interpreting CGM data can be challenging as it reflects a diverse set of complex factors including diet, exercise, sleep, hormones, stress, medications, and any of the other factors that may impact blood glucose levels in a particular person.5 Additionally, different sensors and sensor placement can affect readings, making interpretation difficult at times. For example, sensors placed on the leg reported lower values than those placed on the upper arm during rest.13 Even so, CGM may be a useful tool for monitoring and optimizing glucose balance and recovery in athletes, potentially guiding timely adjustments in nutrition and training for peak performance.
Benefits of Continuous Glucose Monitoring for Athletes
Several studies have investigated the role of CGM in athletes and found that many endurance athletes exhibit hyperglycemia and glucose variability.14-16 These studies have also demonstrated high variability among individuals and indicated that many athletes spend a significant amount of time in a hypo- or hyper-glycemic state.5
CGM offers athletes the ability to better understand blood glucose levels during exercise and make appropriate changes to prevent hypoglycemia or hyperglycemia.5 Because blood glucose levels can remain elevated for up to 24 hours after prolonged exercise, CGM allows optimization of meals, including timing and composition, although this is not always a simple calculation.5
CGM may also help with recovery efforts as it allows athletes to analyze glucose values and trends for 24 hours, including during the night. Hypoglycemia during the night can disrupt sleep which has a negative effect on recovery or possibly the next day’s training session.5 Specifically, when blood glucose levels fall below 50 mg/dL (2.8 mmol/L), it results in the release of epinephrine which triggers wakening.5
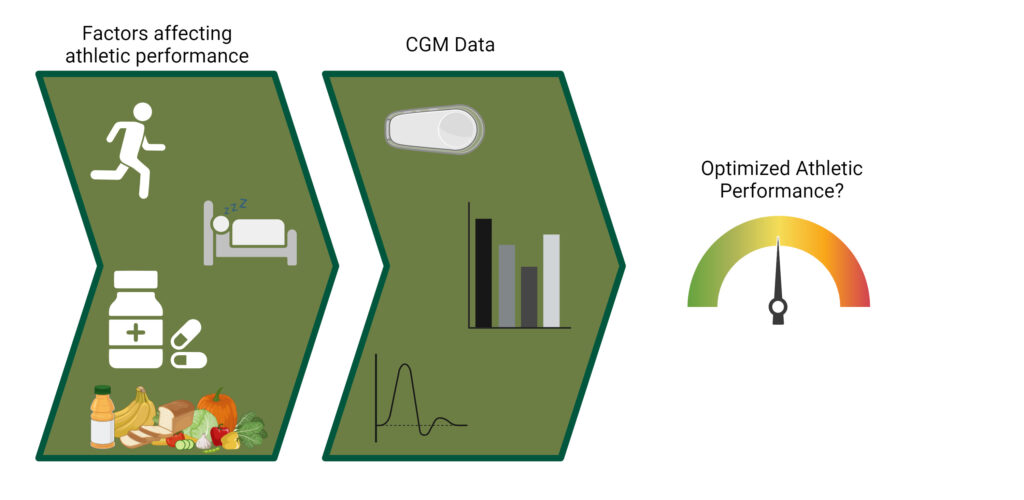
Image created with Biorender.com
Special Considerations for Continuous Glucose Monitoring
It is important to consider individual factors that affect blood glucose levels, including medication use, and exercising timing, which may impact blood glucose in some people.17 Additionally, blood glucose levels can be impacted by overall energy intake. In some athletes, low energy intake or availability— a condition called relative energy deficiency — induces hormonal changes that negatively affect sports performance, health measures, and influences gluconeogenesis and glucose metabolism.5 CGM also cannot define the precise dose or type of carbohydrate before or after exercise to optimize performance.7
Working with a sports nutritionist or holistic healthcare provider can help athletes understand the body’s natural response to various types of exercise, efficiently utilize data from CGM readings in the context of athletic performance and help solidify healthy eating patterns to optimize athletic performance.
Did you know Wholistic Matters is powered by Standard Process? Learn more about Standard Process’ whole food-based nutrition philosophy.
- Campos, C. (2012). Chronic hyperglycemia and glucose toxicity: pathology and clinical sequelae. Postgrad Med, 124(6):90.
- Brun, J.F., Dumortier, M., Fedou, C., Mercier, J. (2001). Exercise hypoglycemia in nondiabetic subjects. Diabetes Metab, 27:92.
- Hirata, Y., Nomura, K., Senga, Y., Okada, Y., Koboyashi, K., et al. (2019). Hyperglycemia induces skeletal muscle atrophy via a WWP1/KLF15 axis. JCI Insight, 4(4):e124952.
- Peinado, A.B., Rojo-Tirado, M.A., Benito, P.J. (2013). Sugar and physical exercise: the importance of sugar for athletes. Nutr Hosp, 28(Suppl 4):48.
- Flockhart, M., Larsen, F.J. (2023). Continuous Glucose Monitoring in Endurance Athletes: Interpretation and Relevance of Measurements for Improving Performance and Health. Sports Med, 54:247.
- Zaharieva, D.P., Riddell, M.C. (2015). Prevention of Exercise-Associated Dysglycemia: A Case Study-Based Approach. Diabetes Spectr, 28(1):55.
- Bowler, A.-L.M., Whitfield, J., Marshall, L., Coffey, V.G., Burke, L.M., Cox, G.R. (2023). The Use of Continuous Glucose Monitors in Sport: Possible Applications and Considerations. Int J Sport Nutr Exerc Metab, 33:121.
- Adams, O.P. (2013). The impact of brief high-intensity exercise on blood glucose levels. Diabetes Metab Syndr Obes, 6:113.
- Kirwan, J.P., Sacks, J., Nieuwoudt, S. (2017). The essential role of exercise in the management of type 2 diabetes. Cleve Clin J Med, 84(7 Suppl 1):S1.
- Hawley, J.A., Hargreaves, M., Zierath, J.R. (2006). Signalling mechanisms in skeletal muscle: role in substrate selection and muscle adaptation. Essays Biochem, 42:1.
- Marliss, E.B., Vranic, M. (2002). Intense exercise has unique effects on both insulin release and its roles in glucoregulation: implications for diabetes. Diabetes, 51(Suppl 1):S271.
- Flockhart, M., Tischer, D., Nilsson, L.C., Blackwood, S.J., Ekblom, B., Katz, A., et al. (2023). Reduce glucose tolerance and insulin sensitivity after prolonged exercise in endurance athletes. Acta Physiol, 238(4):e13972.
- Coates, A.M., Cohen, J.N., Burr, J.F. (2023). Investigating sensor location on the effectiveness of continuous glucose monitoring during exercise in a non-diabetic population. Eur J Sport Sci, 23:1.
- Flockhart, M., Nilsson, L.C., Tais, S., Ekblom, B., Apro, W., Larsen, F.J. (2021). Excessive exercise training causes mitochondrial functional impairment and decreases glucose tolerance in healthy volunteers. Cell Metab, 33(5):957.
- Thomas, F., Pretty, C.G., Desaive, T., Chase, J.G. (2016). Blood glucose levels of subelite athletes during 6 days of free living. J Diabetes Sci Technol, 10(6):1335.
- Prins, P.J., Noakes, T.D., Buga, A., D’Agostino, D.P., Volek, J.S., Buxton, J.D., et al. (2023). Low and high carbohydrate isocaloric diets on performance, fat oxidation, glucose and cardiometabolic health in middle age males. Front Nutr, 10:1084021.
- Savikj, M., Gabriel, B.M., Alm, P.S., Smith, J., Caidahl, K., Bjornholm, M., et al. (2019). Afternoon exercise is more efficacious than morning exercise at improving blood glucose levels in individuals with type 2 diabetes: a randomised crossover trial. Diabetologia, 62:233.