The Impact of Circadian Rhythm on Cortisol and Blood Glucose Levels
Cortisol and its Role in the Body
Cortisol is the body’s stress response hormone but also regulates many different systems and processes in the body, including metabolism, electrolyte balance, cognition, and immune function.1 It also has both direct and indirect effects on blood glucose homeostasis.
Cortisol prompts the liver to release glycogen into the bloodstream which increases blood glucose levels transiently and provides immediate energy to the body.2 It also opposes the actions of insulin, resulting in decreased insulin sensitivity in various tissues in the body, including muscle and fat tissues. These actions work to maintain plasma glucose for brain function during stressful times, however, chronically elevated cortisol can result in hyperglycemia and contribute to the development of insulin resistance and type 2 diabetes.2,3
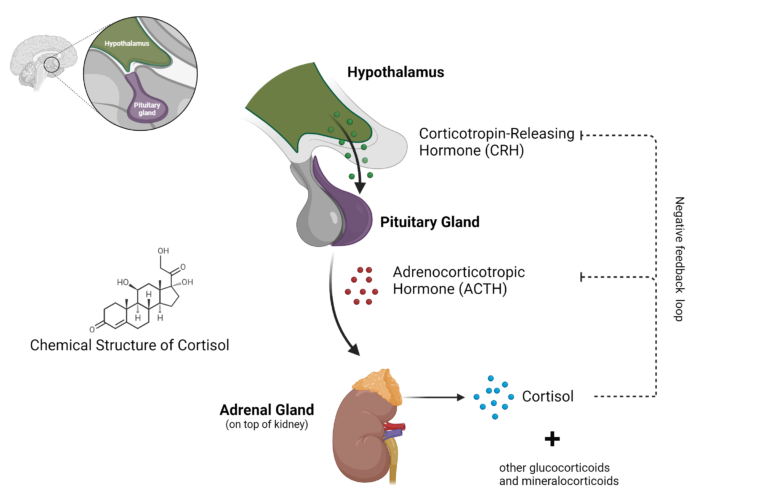
Image created with BioRender.com
Overview and Significance of Blood Glucose Levels
Blood glucose provides energy to cells in the body and contributes to the healthy functioning of many organs. Blood glucose levels are tightly regulated by the hormones insulin and glucagon, both of which are produced by the pancreas.
This regulation is essential for life; high and low blood sugar can significantly harm the body. High blood sugar, or hyperglycemia, can result in excessive thirst, frequent urination, blurred vision, and metabolic disturbances. Hypoglycemia, or low blood sugar, can result in excess hunger, sweating, nausea, headache, and loss of consciousness if severe.
While insulin and glucagon are major regulators of blood glucose levels, many other factors influence glucose homeostasis. Physical activity, sleep, illness, and certain medications can influence glucose metabolism, potentially contributing to dysregulated levels. Stress is a major determinant of blood glucose levels through the actions of cortisol on glucose metabolism. Considering these factors when monitoring and managing blood glucose levels is crucial for optimal well-being.
How Cortisol Affects Blood Glucose Levels
Cortisol is a type of glucocorticoid, a class of steroid hormones originally named because of their effects on glucose levels.2 In the liver, cortisol and other glucocorticoids promote gluconeogenesis, converting non-glucose compounds into glucose.2 However, in skeletal muscle and white adipose tissue, they decrease glucose uptake and utilization by opposing the effects of insulin.2 Together, this results in a state of hyperglycemia and insulin resistance.
Cortisol can also directly affect the function of alpha and beta cells in the pancreas, which secrete glucagon and insulin, respectively.2 Other effects of cortisol include regulating lipid mediators that contribute to insulin sensitivity and glucose utilization and promoting lipolysis in white adipose tissue which impairs glucose homeostasis via the aberrant signaling of diacylglycerol and ceramides.2
Understanding the Relationship Between Circadian Rhythm and Cortisol Levels
The body contains an internal clock that follows a pattern that takes about 24 hours to complete. This 24-hour pattern, or circadian rhythm, synchronizes light-dark cycles with many physiological processes in the body.1 The master clock of the body is found in the suprachiasmatic nucleus (SCN) in the hypothalamus and coordinates the rhythm of bodily processes with peripheral clocks in nearly every organ and cell.1,4
The hypothalamus plays a key role in both circadian rhythm as the location of the master clock of the body and as a regulator of cortisol production. It releases CRH which signals the pituitary gland to release ACTH which then stimulates the adrenal glands to produce cortisol. In addition to its many other functions, cortisol is an important component of the body’s circadian rhythm, signaling in nearly every tissue in the body and dictating the cycle of many biological functions.1
How Your Body’s Internal Clock Affects Cortisol Production
Cortisol contributes to the circadian rhythm in peripheral tissues but also follows its own cycle of increasing and decreasing levels.1 The circadian clock of the adrenal glands results in specific timeframes where the adrenal glands are more responsive to ACTH, and therefore produce and release more cortisol.5 Interestingly, clock gene expression varies between different areas of the adrenal gland, indicating a high degree of circadian regulation of the adrenal glands.5
Cortisol exhibits four distinct periods of circadian rhythm in healthy individuals over the course of a day. Secretion is minimal in the two to four hours after the onset of sleep.5 After this period, there is mild secretion, followed by the third phase of increasing cortisol production during the sixth through eighth hours of sleep.5 This elevated cortisol secretion continues through the first hour of waking and is followed by intermittent periods of activity during the waking period .5
Because the body also responds to environmental and behavioral cues as well as circadian rhythm, there is variation in these phases between individuals.5
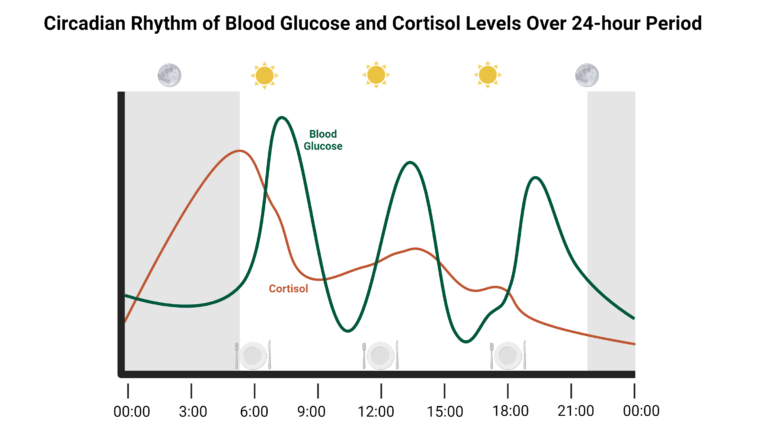
Image created with BioRender.com
Influence of Circadian Rhythm Disruptions on Blood Glucose Levels
Organs and body systems follow their own circadian rhythm. This includes the liver, which is a major regulator of blood glucose levels, and the pancreas, which synthesizes insulin and glucagon. As such, disturbances in circadian rhythm in either of these organs can lead to dysregulated blood glucose levels.6 For example, disruptions of circadian rhythm in pancreatic beta cells result in impaired insulin secretion and changes in beta cell proliferation and survival, increasing the risk of developing type 2 diabetes.6
Circadian rhythm disturbances are commonly seen in night shift workers, resulting in changes in hormone secretion, food intake, and energy expenditure.6 To help minimize the adverse effects of circadian rhythm disruptions on blood glucose levels, it is important to maintain a consistent sleep routine and practice healthy sleep hygiene habits.
Exploring the Link Between Circadian Rhythm and Blood Sugar Spikes
While carbohydrate intake is the primary determinant of blood glucose levels, glucose homeostasis follows a circadian rhythm, especially during fasting periods.6 The SCN in the hypothalamus as well as peripheral clocks in the liver, pancreas, muscle, and white adipose tissue play an important role in maintaining blood glucose homeostasis.6 If circadian rhythm is disrupted due to irregular sleep patterns or shift work, it can lead to the dysregulation of blood sugar and increase the risk of metabolic disorders through direct and indirect mechanisms.
The central biological clock influences blood glucose levels in a variety of ways, including glucose production, glucose uptake, insulin release, and insulin sensitivity.6 Using animal models that lack important circadian rhythm genes, scientists have found that when the body loses its circadian rhythm it results in detrimental changes to body weight, white adipose tissue mass, glucose levels, glucose tolerance, insulin levels, insulin sensitivity, and lipid levels.6
Changes in circadian rhythm can also alter eating habits, which can further contribute to insulin resistance. The body also naturally produces more glucose right before waking, but when this process is dysregulated, it can lead to improperly elevated blood glucose levels that do not align with other rhythmic functions in the body.6,7
Cortisol is a key link between circadian rhythm and blood glucose metabolism. Hypercortisolism promotes dysregulated glucose metabolism by promoting the accumulation of visceral white adipose tissue, increasing gluconeogenesis, impairing insulin signaling in skeletal muscle, and promoting lipolysis which releases free fatty acids that disrupt normal cellular signaling.3,8 Cortisol also regulates the liver, which plays a key role in maintaining blood glucose levels.6 As such, disturbances in cortisol can lead to spikes in blood glucose levels.6
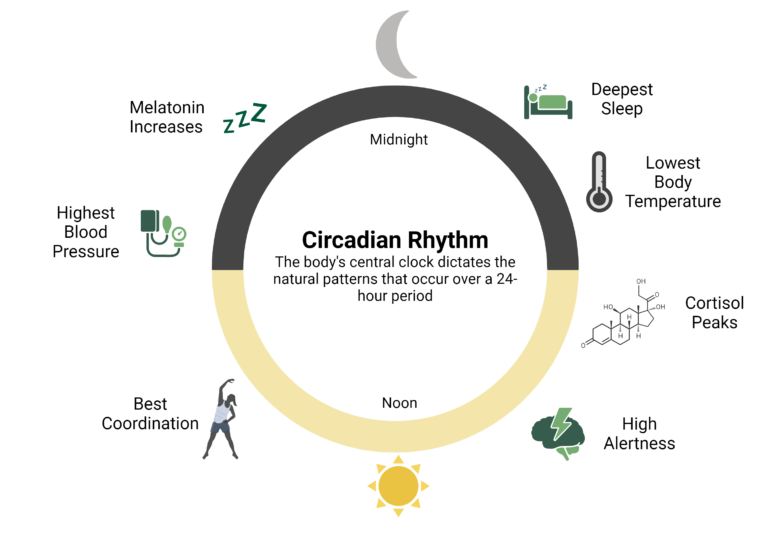
Image created with BioRender.com
Strategies for Stabilizing Blood Glucose by Supporting Circadian Rhythm
Because circadian rhythm can directly and indirectly influence blood glucose levels, maintaining a regular circadian rhythm is important. Following a consistent, daily routine of waking and going to sleep can keep the body’s circadian rhythm steady because light is a major regulator of the master clock in the brain. Creating a healthy sleep environment can also promote quality sleep, which, in turn, promotes a regular circadian rhythm. Additionally, data supports the ability of light to control the master clock.9
Exposure to natural sunlight in the first hour of waking and reducing exposure at night can reset the body’s internal clock and keep it on a 24-hour cycle. Morning light exposure has been found to improve circadian rhythm, sleep quality, and mood.9
Managing stress can also help support healthy blood glucose levels and circadian rhythm. Stress impairs many processes in the body, including HPA axis activity and circadian clocks in the brain.10
The body’s ability to respond to stress via the HPA axis also depends on the time of day, highlighting the complex connection between stress and circadian rhythm. Because of this, it is critical to maintain cortisol levels in a healthy range to help stabilize the body’s circadian rhythm and support healthy blood glucose levels. Engaging in stress management techniques, such as meditation, can help reduce cortisol levels.11
Lifestyle Factors Impacting Cortisol and Blood Glucose Levels
Many lifestyle factors impact blood glucose and cortisol levels including stress, physical activity, and diet. Physical activity supports healthy blood glucose metabolism, increases insulin sensitivity, and decreases stress which reduces cortisol.12 Engaging in regular physical activity has the added benefit of promoting sleep.12 Similarly, healthy food choices positively impact both cortisol and blood glucose.
Healthy, nutrient-dense foods can contribute to healthy inflammation, oxidative balance, gut microbiome diversity, and healthy immune function. All of these contribute to the health of organs in the body, including the hypothalamus, adrenal glands, and pancreas. Timing meals appropriately also promotes a healthy circadian rhythm, aligning with natural cycles in the body to help keep cortisol and blood glucose in a healthy range.
Diet and Nutrition Tips for Cortisol and Blood Sugar Management
Consuming a healthy diet supports healthy cortisol and blood glucose levels. Choosing nutrient-dense, whole foods can promote a healthy inflammatory response in the adrenal glands and pancreas. Because inflammation negatively affects the pancreas, damaging beta cells and disrupting insulin secretion, supporting the resolution of inflammation can help maintain normal production of insulin, which helps keep blood glucose levels in a healthy range.13
Consuming complex carbohydrates with lean proteins and healthy fats results in a much lower blood glucose peak compared to simple, easily digestible carbohydrates.14
In addition to optimizing meal composition, timing meals with the body’s circadian rhythm helps keep systems synchronized and can also support healthy blood glucose metabolism. Aligning meals with the body’s hunger and satiety cues also helps inhibit excessive caloric intake. This further strengthens the body’s natural circadian rhythm and prevents overeating which can contribute to a spike in blood glucose.
Specific nutrients can help support cortisol balance, including vitamin C and several B vitamins which are used in the production of cortisol. Omega-3 fatty acids can decrease cortisol levels as well as perceived feelings of stress.15, 16 Additionally, clinical studies have confirmed that stress can deplete levels of essential minerals including magnesium, calcium, and zinc.17 Choosing whole-food or supplemental sources of these minerals can normalize stores in the body, supporting the many physiological processes that require magnesium, calcium, and zinc.
The Impact of the Mediterranean Diet on Cortisol and Blood Glucose
For patients who struggle to track intake of specific micronutrients, following a dietary pattern can be easier and lead to better results. The Mediterranean Diet (MedDiet) is a dietary pattern that supports blood glucose, cortisol homeostasis, healthy inflammation, and a diverse gut microbiome. This diet is rich in micronutrients that are required for hormone production and a range of other physiological processes.
Many studies have also demonstrated the ability of the MedDiet to protect against health issues including diabetes, excess cortisol levels, and poor sleep quality.18-21 The MedDiet is also rich in melatonin which is another key regulator of circadian rhythm.22
Circadian rhythm, cortisol physiology, and blood glucose metabolism are complex, interconnected processes. As such, they require a holistic approach to properly manage. Engaging in regular physical activity, consuming macronutrients in balanced proportions and micronutrients that are susceptible to stress-induced depletion, as well as managing stress can promote the health of all these systems and components.
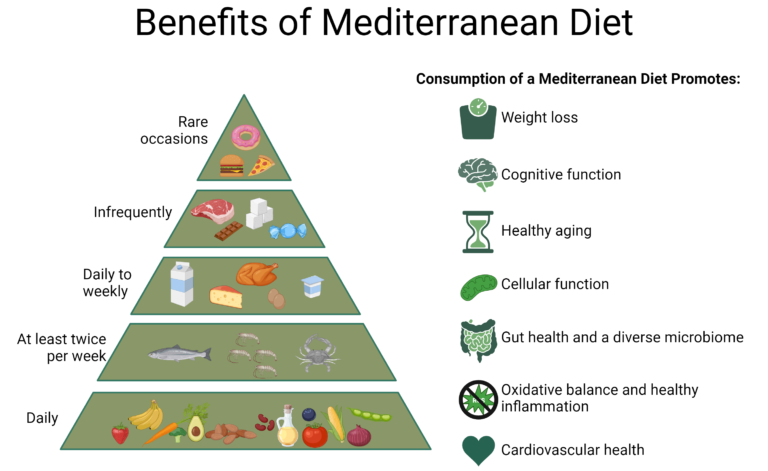
Image created with BioRender.com
Did you know Wholistic Matters is powered by Standard Process? Learn more about Standard Process’ whole food-based nutrition philosophy.
- Azmi, N.A.S.M., Juliana, N., Azmani, S., Effendy, N.M., Abu, I.F., Teng, N.I.M.F., Das, S. (2021). Cortisol on Circadian Rhythm and Its Effect on Cardiovascular System. J Environ Res Public Health, 17:0.
- Kuo, T., McQueen, A., Chen, T.-C., Wang, J.-C. (2015). Regulation of Glucose Homeostasis by Glucocorticoids. Adv Exp Med Biol, 872:99.
- Ortiz, R., Kluew, B., Odei, J.B., Tcheugui, J.B.E., Sims, M., Kalyani, R.R., et al. (2019). The association of morning serum cortisol with glucose metabolism and diabetes: The Jackson Heart Study. Psychoneuroendocrinology, 103:25.
- Mason, I.C., Qian, J., Adler, G.K., Scheer, F.A.J.L. (2020). Impact of circadian disruption on glucose metabolism: implications for type 2 diabetes. Diabetologia, 63(3):462.
- Chan, S., Debono, M. (2010). Replication of cortisol circadian rhythm: new advances in hydrocortisone replacement therapy. Ther Adv Endocrinol Metab, 1(3):129.
- Kalsbeek, A., le Fleur, S., Fliers, E. (2014). Circadian control of glucose metabolism. Mol Metab, 3(4):372.
- Bolli, G.B., Gerich, J.E., 1984. The “Dawn-Phenomenon” — a common occurrence in both non-insulin-dependent and insulin-dependent diabetes mellitus. N Engl J Med, 310(12):746.
- Khani, S., Tayek, J.A. (2011). Cortisol increases gluconeogenesis in humans: its role in the metabolic syndrome. Clin Sci (Lond), 101(6):739.
- Blume, C., Garbazza, C., Spitschan, M. (2019). Effects of light on human circadian rhythms, sleep and mood. Somnologie (Berl), 23(3):147.
- Koch, C.E., Leinweber, B., Drengberg, B.C., Blaum, C., Oster, H. (2017). Interaction between circadian rhythms and stress. Neurobiol Stress, 6:57.
- Turakitwanakan, W., Mekseepralard, C., Busarakumtragul, P. (2013). Effects of mindfulness meditation on serum cortisol of medical students. J Med Assoc Thai, 96 Suppl 1:S90.
- De Nys, L., Anderson, K., Ofosu, E.F., Ryde, G.C., Connelly, J., Whittaker, A.C. (2022). The effects of physical activity on cortisol and sleep: A systematic review and meta-analysis. Psychoneuroendocrinology, 143:105843.
- Cerf, M.E. (2013). Beta Cell Dysfunction and Insulin Resistance. Front Endocrinol, 4:37.
- Holesh, J.E., Aslam, S., Martin, A. Physiology, Carbohydrates. [Updated 2023 May 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459280/.
- Stachowicz, M., Lebiedzinska, A. (2016). The effect of diet components on the level of cortisol. European Food Research and Technology, 242:2001.
- Barbadoro, P., Annino, I., Ponzio, E., Romanelli, R.M., D’Errico, M.M., Prospero, E., Minelli, A. (2013). Fish oil supplementation reduces cortisol basal levels and perceived stress: a randomized, placebo-controlled trial in abstinent alcoholics. Mol Nutr Food Res, 57(6):1110.
- Lopresti, A.L. (2020). The Effects of Psychological and Environmental Stress on Micronutrient Concentrations in the Body: A Review of the Evidence
- Martin-Pelaez, S., Fito, M., Castaner, O. (2020). Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients, 12(8):2236.
- Carvalho, K.M.B., Ronca, D.B., Michels, N., Huybrechts, I., Cuenca-Garcia, M., Marcos, A., et al. (2018). Does the Mediterranean Diet Protect against Stress-Induced Inflammatory Activation in European Adolescents? The HELENA Study. Nutrients, 10(11):1770.
- Alufer, L., Tsaban, G., Rinott, E., Kaplan, A., Meir, A.Y., et al. (2023). Long-term green-Mediterranean diet may favor fasting morning cortisol stress hormone; the DIRECT-PLUS clinical trial. Front Endocrinol, 14:1243910.
- Godos, J., Ferri, R., Lanza, G., Caraci, F., Vistorte, A.O.R., Torres, V.Y., et al. (2024). Mediterranean Diet and Sleep Features: A Systematic Review of Current Evidence. Nutrients, 16(2):282.
- Grao-Cruces, E., Calvo, J.R., Maldonado-Aibar, M.D., Millan-Linares, M.C., Montserrat-de la Paz, S. (2023). Mediterranean Diet and Melatonin: A Systematic Review. Antioxidants (Basel), 12(2):264.







