Nutrition, Lifestyle, and Exercise for Optimal Cardiovascular Health
Cardiovascular disease (CVD) is characterized as a group of disorders impacting the heart and blood vessels including congestive heart failure, coronary heart disease, cardiomyopathy, and atherosclerosis. CVD is the leading cause of death globally, contributing to over 30% of reported deaths with an estimated annual cost of $252 billion.1
Cardiovascular Health Defined
The cardiovascular system, comprising the heart and blood vessels, is responsible for circulating blood throughout the body. In addition, this system facilitates the transport of nutrients, exchange of gases, and the excretion of waste from the blood and body. There are two specific pathways within the cardiovascular system: pulmonary circulation and systemic circulation. Pulmonary circulation ensures the oxygenation of blood, while systemic circulation delivers oxygenated blood, and nutrients, to the rest of the body.
The heart is a muscle that serves as the primary pump for blood circulation. It is composed of four chambers and four valves, which ensures that deoxygenated blood is pumped to the lungs, and oxygenated blood is pumped to every other area of the body. Each heartbeat propels the blood further through the arteries, arterioles, capillaries, and veins.
Arteries are the first vessels to carry oxygenated blood away from the heart to the rest of the body. They divide into smaller arteries, and arterioles, which act as secondary pumps by contracting or relaxing to control blood flow. Arterioles flow into capillaries, which are the width of a single red blood cell which allows for the efficient exchange of nutrients, oxygen, carbon dioxide and waste with body tissues. As blood is used, or deoxygenated, it will be delivered back to the heart via veins, and the process starts all over again.
The heart is continuously adapting to the demands of the body. An increased demand for oxygenated blood can be signaled by the lungs, kidneys, liver, or skin, causing the heart to beat faster and increase output. Stimuli from hormones, the nervous system, electrolytes or drugs can have an impact as well, but exercise is a prime example of adaptation that becomes more efficient over time. 2
When an individual begins exerting energy towards exercise, they notice an immediate rise in their heart rate. This is due to the increased needs for oxygenated blood to the muscles and throughout the body, signaling the heart to pump more efficiently. The cardiovascular system is very effective at adapting to a stimulus. When participating in repeated exercise over a period, the will begin responding differently to said stimulus where the heart doesn’t have to beat as rapidly. This is a result of training the heart muscle to work more efficiently in response to stimulus, or through exercise. As a result, exercise is one of the most important aspects, along with a healthy diet, of keeping your cardiovascular system healthy.
The health of your cardiovascular system is influenced by a multitude of factors, including your diet, lifestyle choices, environment, stress, and genetic factors. For example, a diet high in saturated fats and excess alcohol can increase your risk of cardiovascular disease.3
Modifiable Risk Factors for Cardiovascular Concerns
The Centers for Disease Control estimates that 47% of Americans have 1 of 3 key factors for cardiovascular disease, which include high blood pressure, high cholesterol, or smoking. There are additional risk factors including your age, lifestyle habits, adjunctive health conditions, and genetic factors.
As cardiovascular disease is an overarching condition impacting the whole of the cardiovascular system, there are certain conditions or physiological abnormalities that can increase your risk for development of CVD:
- High blood pressure – increased pressure from the blood within blood vessels is too high.
- High cholesterol levels – excess cholesterol levels in the body can build up on the walls of the arteries, blocking the flow of blood to major organs.
- Diabetes – alterations in glucose metabolism can be a risk factor for the development of cardiovascular disease.
- Obesity – those carrying extra body fat are at a higher risk of heart disease or stroke, as well as cardiovascular disease risk factors.
- Plaque build-up – atherosclerotic plaque can thin the arterial walls, leading to increased cardiovascular risk concerns.
- Genetic factors – genetic factors are those that are difficult to modify by diet or lifestyle and can contribute to your risk of developing cardiovascular disease.
Additionally, there are modifiable risk factors that contribute to the development or an increased risk of cardiovascular disease. These are risk factors that some individuals might participate in during day-to-day life that can easily be changed or improved to decrease the risk of cardiovascular disease. These modifiable risk factors include:
- Excess alcohol consumption
- Inactivity
- Tobacco and smoking
- Excess saturated and/or trans-fat consumption
- Overweight or extra bodyweight
- Inadequate consumption of vegetables & fruits
Over 90% of risk factors for cardiovascular disease are modifiable risk factors, or conditions that could be improved through modifying lifestyle habits.4 With simple changes, individuals are able to significantly reduce their risk of cardiovascular disease and improve cardiovascular health!
Nutrition to Improve Cardiovascular Health
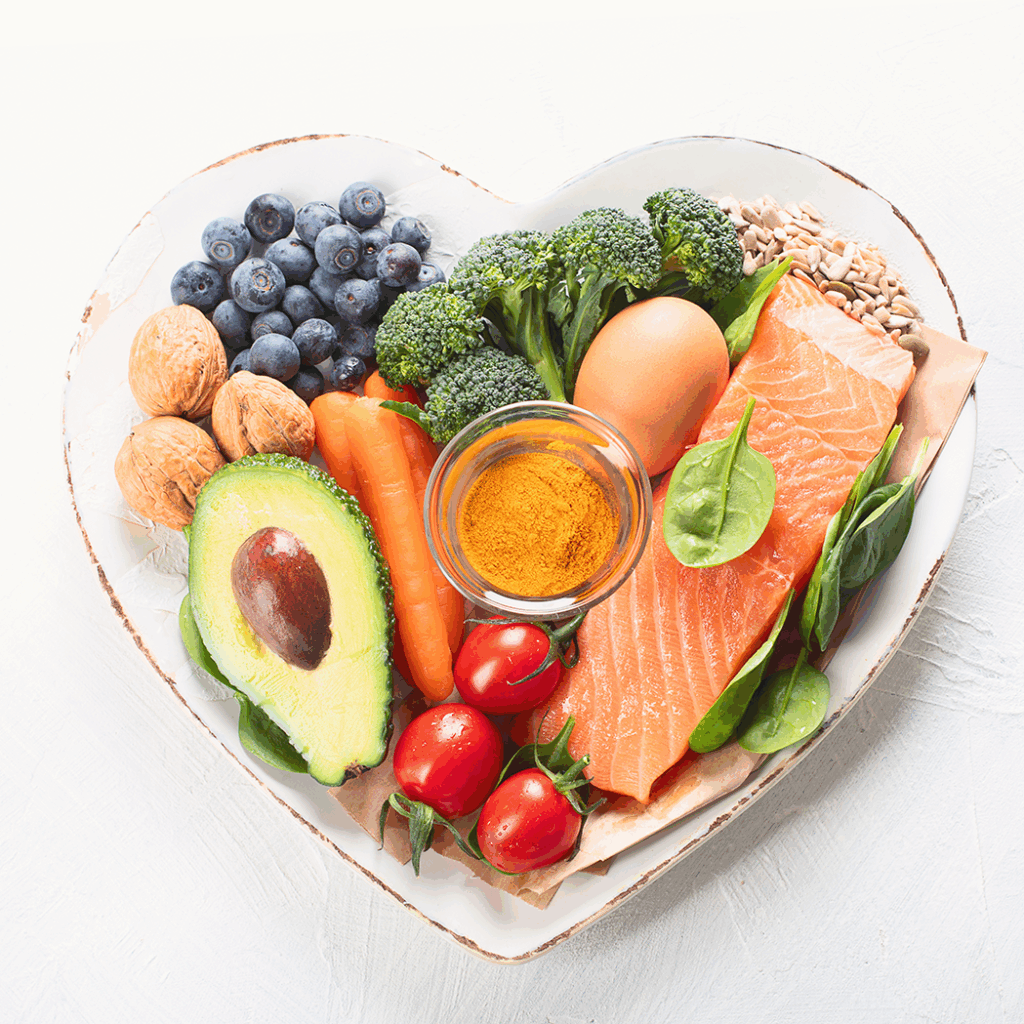
A healthy diet is one of the most influential, modifiable factors that can improve cardiovascular health status. In some cases, implementing a heart healthy diet has reversed heart disease and significantly decreased cardiovascular risk factors.5 A heart healthy diet is one rich in lean proteins, fruit, vegetables, fiber, nuts, seeds, quality whole grains, and water. Current research suggests the Mediterranean, DASH, and plant-based diets have the most influential cardioprotective effects on cardiovascular disease, and cardiovascular risk factors.6 Below is a review to highlight why these nutrients within a dietary intervention improve cardiovascular health.
Protein
Protein is one of the three macronutrients. Protein is composed of amino acids, which provide nutrients for muscle building and muscle repair, provide energy, and are essential for a healthy heart. Protein is found in an abundance of heart healthy foods like chicken, yogurt, fish, legumes, nuts, seeds, seafood, eggs, and lean red meat. The American Heart Association recommends a higher amount of chicken and fish, averaging at least two to three servings per week, for a heart healthy diet as these protein sources have shown the greatest benefit to reducing cardiovascular risk.7 Protein also plays a role in regulating blood glucose and blood sugar levels, which further can reduce risk of cardiovascular disease.8
Fruits and Vegetables
Nutrition professionals will all stress the importance of consuming more color, more flavor, and more diversity in the diet to reduce your risk of developing disease or reducing your risk of disease development. Fruits and vegetables contain heart healthy compounds like fiber, vitamins, minerals, and phytonutrients that you can only consume through plants. Phytonutrients play a large role in reducing your risk of cardiovascular disease by providing antioxidants to improve your overall health status.
Omega-3s or Dietary Fats
Dietary fats include sources of nuts, seeds, oils, avocados, and flaxseeds are excellent sources of heart healthy nutrients. For cardiovascular health, dietary fats rich in monounsaturated fats and polyunsaturated fats have been linked to improvements in heart health, like a reduction of plaque buildup within the arteries.9 Additionally, Omega-3’s, which is a compound found in dietary fats, are beneficial at reducing your risk of cardiovascular disease because they promote heart health. Omega-3’s have been studied to reduce cardiovascular mortality, inhibit inflammation, and reduce blood pressure.10 Omega-3’s can also be found in fish, which provide you with the benefit of lean protein and quality dietary fats.
Whole Grains
While an excess consumption of carbohydrates can contribute to cardiovascular disease, carbohydrates from whole grains are essential for overall health. Carbohydrates provide dietary fiber and a deficiency in dietary fiber has been linked to a significantly increased risk factor for cardiovascular disease. Dietary fiber is a foundational part of plants and serves as an agent to reduce high blood pressure, high blood sugar, diabetes, cholesterol levels, and reduce the risk of atherosclerotic plaque development. Additionally, dietary fiber helps modulate a healthy gut microbiome, which could influence risk of cardiovascular disease.11 Carbohydrates from sweet potatoes, fruits, vegetables, squash, rice, quinoa, oatmeal, legumes, and beans would be considered heart healthy sources. To promote cardiovascular health, individuals should limit those carbohydrates that are ultra-processed, refined, and rich in sugar.
Exercise and Cardiovascular Health

While diet is one of the best modulators of healthy cardiovascular health, exercise comes in as a great adjunctive therapy to improve cardiovascular health. The development of cardiovascular disease is directly related to inactivity. Exercise acts as a stimulus to the heart, which keeps the cardiovascular system active, moving, and adaptive to changes, while improving overall circulatory function. Inactivity results in regression of the heart muscle as there is no longer a stimulus to continuously challenge the muscle, this regression leads to an increase in cardiovascular disease risk.
To prevent cardiovascular concerns, the American Heart Assocation recommends a minimum of 150 minutes of exercise per week coming from moderate to intense aerobic session, or 75 minutes of high-intensity aerobic exercise.12 The importance of exercise is finding something enjoyable, but it is challenging to continuously train the heart muscle.
Additionally, exercise has direct impacts on lowering factors associated with cardiovascular disease risk. For example, atherosclerosis is a factor we discussed in earlier paragraphs contributing to cardiovascular disease. Exercise has a direct effect on atherosclerosis by promoting the reduction of atherosclerotic plaque buildup.13 Or excess adipose tissue contributes to cardiovascular disease risk, and exercise can help increase calories burn which can result in weight loss. Exercise can also help reduce LDL cholesterol, while improving HDL cholesterol, which is another direct cardiovascular disease factor.
Cardiovascular Health Outcomes
When discussing cardiovascular health, the changes made with nutritional interventions and changing lifestyle habits can be influential in reducing your risk of cardiovascular disease in the long run. The most important factors are consuming a healthy diet and ensuring participation in regular exercise to get the heart pumping! The changes made today are the changes that will influence cardiovascular health in the future.
Did you know Wholistic Matters is powered by Standard Process? Learn more about Standard Process’ whole food-based nutrition philosophy.
- The World Health Organization. (2021). Cardiovascular Diseases (CVDs) [Fact sheet]. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- McGarrah, R. W., Crown, S. B., Zhang, G., Shah, S. H., Newgard, C. B. (2019). Cardiovascular Metabolomics. Circulation Research, 122(9), 1238-1258.
- The Centers for Disease Control and Prevention. (2024). Heart Disease Risk Factors. https://www.cdc.gov/heart-disease/risk-factors/index.html
- Rezaianzadeh, A., Moftakhar, L., Seif, M., Johari, M. G., Hosseini, S. V., Dehghani, S. (2023). Incidence and Risk Factors of Cardiovascular Disease among Populations aged 40-70 years: A Population-Based Cohort Study in the South of Iran. Tropical Medicine and Health, 51(35).
- Yu, E., Malik, V. S., Hu, F. B. (2019). Cardiovascular Disease Prevention by Diet Modification: JACC Health Promotion Series. Journal of the American College of Cardiology, 72(8), 914-926.
- Diab, A., Dastmalchi, L. N., Gulati, M., Michos, E. D. (2023). A Heart-Healthy Diet for Cardiovascular Disease Prevention: Where Are We Know? Vascular Health and Risk Management, 19, 237-253.
- American Heart Association. (2024). Picking Healthy Proteins. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/picking-healthy-proteins
- Gannon, M. C., Nuttall, F. Q., Saeed, A., Jordan, K., Hoover, H. (2003). An Increase in Dietary Protein Improves the Blood Glucose Response in Persons with Type 2 Diabetes. American Journal of Clinical Nutrition, 78(4), 734-741.
- Sacks, F. M., Lichtenstein, A. H., Wu, J. H. Y., Appel, L. J., Creager, M. A., Kris-Etherton, P. M., Miller, M., Rimm, E. B., Rudel, L. L., Robinson, J. G., Stone, N. J., Van Horn, L. V. (2017). Dietary Fats and Cardiovascular Disease: A Presidential Advisory from the American Heart Association. Circulation, 126(3), e1-e23.
- Li, J. J., Dou, K. F., Zhou, Z. G., Zhao, D., Ye, P., Zhao, J. J., Guo, L. X. (2022). Role of Omega-3 Fatty Acids in the Prevention and Treatment of Cardiovascular Diseases: A Consensus Statement from the Experts’ Committee of National Society of Cardiometabolic Medicine. Frontiers in Pharmacology, 13.
- McRae, M. P. (2017). Dietary Fiber is Beneficial for the Prevention of Cardiovascular Disease: An Umbrella Review of Meta-Analyses. Journal of Chiropractic Medicine, 16(4), 289-299.
- American Heart Association. (2024). Recommendations for Physical Activity in Adults and Kids. https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults
Al-Mamari, A. (2009). Atherosclerosis and Physical Activity. Oman Medical Journal, 24(3), 173-178.