Magnesium: The Forgotten Nutrient
Magnesium: The Forgotten Nutrient
Magnesium is an essential nutrient. It enables key metabolic processes, contributes to bone strength, and acts as a cofactor in hundreds of enzymatic reactions.1 Despite its central role in physiology and health, magnesium is under-consumed by most Americans, leading to chronic magnesium deficiency and increased risk for multiple serious health conditions, such as cardiovascular disease, type 2 diabetes, and depression.2 The main factors underlying reduced magnesium intake are the declining nutrient content of produce and refined grains, and increased consumption of processed foods, both of which are common in the Standard American Diet (SAD). Boosting magnesium intake to recommended levels requires people to improve the quality of their diets by increasing consumption of whole foods, reducing intake of processed foods, and possibly using daily magnesium supplements.
This article reviews the central importance of magnesium in the human body, the causes and consequences of magnesium deficiency, and approaches to improve magnesium status and overall health.
Why Is Magnesium Important?
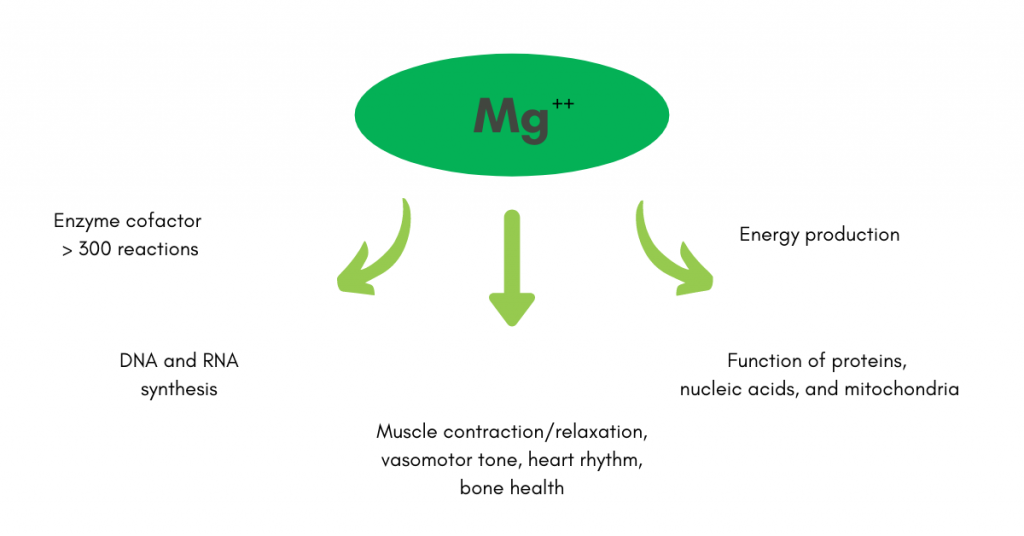
Magnesium is the fourth most abundant cation in the human body. It plays a central role in energy production, glycolysis, and the synthesis of proteins and nucleic acids (DNA and RNA).1 Among other actions, magnesium is a cofactor for more than 300 enzymes and is essential to cell growth and function, energy storage and production, stabilization of cell membranes, nerve conduction, muscle contraction, and the function of ion channels (Figure 1).3-4
Unfortunately, multiple survey studies from the United States, Europe, and other regions have demonstrated that the recommended daily allowance (RDA) of magnesium remains unmet in a large proportion of the population, likely as a result of SAD dietary patterns.5-8 It is estimated that about half of the United States population consumes less than the RDA of magnesium.6,9 The estimated severity of magnesium deficits has led some experts to suggest that many people need greater than 300 milligrams of magnesium per day to replete and maintain body stores.10
How the Body Regulates Magnesium
The average human body contains about 24 grams of magnesium.11 Most magnesium in the body is intracellular, with greater than 90 percent located in bone, muscle, and other soft tissues; serum levels represent only about one percent of total body magnesium stores.10-11 In humans, magnesium is regulated through three key mechanisms: absorption by the gut; renal filtration, reabsorption, and excretion; and exchange with the reservoir of magnesium in bone.10,11 About 25 percent to 75 percent of magnesium consumed in the diet is absorbed by the gut; the degree of absorption depends on multiple factors, most notably magnesium status.11
The kidneys filter about 2.4 grams of magnesium per day, reabsorbing about 95 percent and excreting any excess in the urine.11 When magnesium levels are low, the kidneys increase reabsorption and urinary concentrations fall; when magnesium intake exceeds requirements, the excess magnesium is excreted in the urine. Because magnesium is tightly regulated by the kidneys, urinary magnesium levels are a fairly good indicator of magnesium intake; levels less than 80 mg/d suggest risk for magnesium deficiency.13
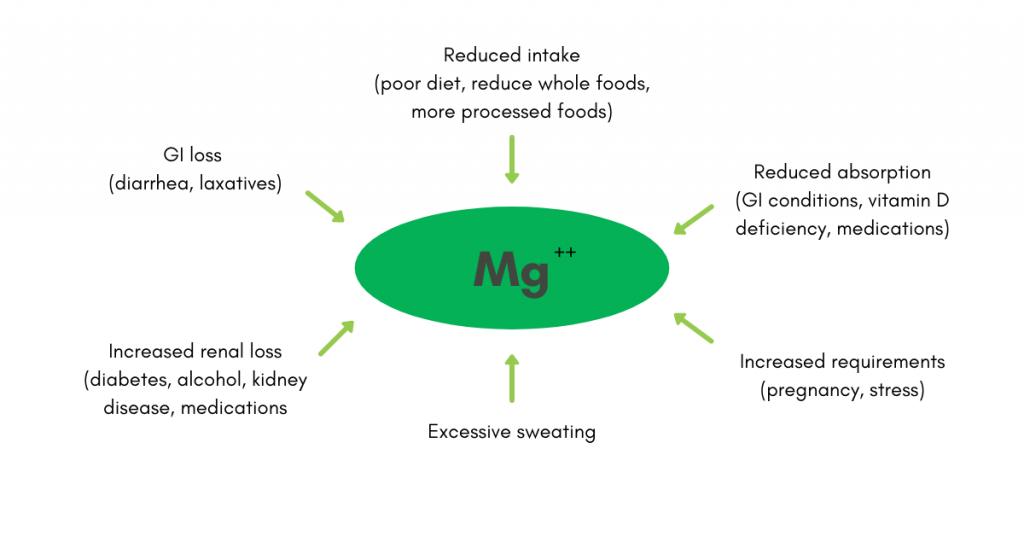
Factors that may contribute to magnesium deficiency include inadequate dietary intake, reduced absorption by the gut, increased losses through the gut or kidney, excessive sweating (e.g., vigorous exercise), increased magnesium needs (e.g., pregnancy, chronic stress), and the effects of certain medications (Figure 2).4,14
When dietary intake and renal reabsorption of magnesium are insufficient to meet physiological needs, magnesium may be mobilized from muscle and bone, potentially contributing to hidden deficits of magnesium.11,12 These hidden or subclinical magnesium deficiencies are especially concerning, as they appear to be common, are difficult to diagnose, and may contribute to a wide range of chronic health problems.15,16 Several sources indicate that up to one-third of the general population has a subclinical magnesium deficiency.9,17 However, the prevalence of subclinical magnesium deficiency may be higher than estimated, as current methods for determining body magnesium levels (e.g., serum, urine, dietary intake) are likely inaccurate.18
Potential Health Consequences of Magnesium Deficiency
Lower magnesium levels have been linked to a broad array of chronic health conditions, ranging from cardiovascular disease to depression (Table 1). Proposed mechanisms through which magnesium may affect risk for chronic diseases include modulation of cellular metabolism and reproduction, systemic inflammation, oxidative stress, thrombosis, and endothelial function, among others.3
Table 1. Studies demonstrating an association between magnesium intake and common diseases.
| Condition | Relation to Magnesium Intake |
| Bone disease |
|
| Depression |
|
| Heart failure |
|
| Hypertension |
|
| Kidney disease |
|
| Metabolic syndrome |
|
| Migraines |
|
| Stroke |
|
| Type diabetes (T2D) |
|
Health Benefits of Higher Magnesium Intake
In contrast to magnesium deficits, higher dietary magnesium intake has been linked to reduced risk for major diseases, reduced stress and depression, and improved migraine symptoms (see Table 1). Higher dietary intake has also been associated with increased fat-free mass (i.e., skeletal muscle), reduced risk for frailty, improved grip strength and bone density, and reduced risk of mortality due to liver disease.40-43 For example, an analysis of the National Health and Nutrition Examination Survey (NHANES) cohort found a 49 percent reduction in risk for mortality due to liver disease for every 100 mg increase in magnesium intake.43
Aging is associated with higher risk for magnesium deficiency due to age-related changes in diet, intestinal absorption, and renal function.44,45 However, adequate magnesium status may support healthy aging not only by reducing risk for the multiple diseases described above, but by preserving chromosomal function. Telomeres are chromosomal structures that contribute to chromosomal integrity and cell health and longevity; reduced telomere length has been linked to age-associated diseases (such as cancer) and mortality.46-47 One study of 10,568 adults from NHANES found that high mineral and vitamin consumption, including magnesium, was associated with increased telomere length, suggesting better cellular integrity.47 Other studies have also identified a link between magnesium status, telomeres, and healthy aging.48
Substantial and mounting evidence, therefore, implicates magnesium deficits in higher risk for multiple serious chronic health conditions, whereas higher magnesium intake reduces health risks and supports normal physiologic function.
How Much Magnesium is Enough?
The proposed normal range for serum magnesium is approximately 1.7 to 2.2 mg/dL.49 The recommended daily allowance (RDA) and estimated average requirement (EAR) to maintain healthy levels of magnesium vary based on age, sex, and reproductive status (Table 2).50-52
Table 2. Estimated average requirements (EAR) and recommended daily allowances (RDA) for magnesium intake in adults.50-52
| Age (years) | EAR (mg/day) | RDA (mg/day) |
| 19-30 (males/females) | 330/255 | 400/310 |
| >30 (males/females) | 350/265 | 420/320 |
| Pregnancy (14-18/19-20/31-50) | 335/290/300 | 400/350/360 |
The Problem: Insufficient Dietary Magnesium Intake
With declining nutrient content in foods and broad consumption of SAD-style diets, deficiencies in essential nutrients such as magnesium have become extremely common. An analysis of 2005-2006 NHANES data identified dietary magnesium intake below EAR in 48 percent of 8437 participants.6 In this study, about 60 percent of surveyed adults did not consume the established RDA for magnesium. A diet-modeling study based on 8944 participants in NHANES (2007-2010) revealed that the percentage of individuals consuming below the EAR for magnesium ranged from 51.7 percent to 88.5 percent for adult males and 34.5 percent to 75.8 percent for adult women.5 Accordingly, the 2015-2020 Dietary Guidelines for Americans designate magnesium as an under-consumed nutrient relative to the EAR in the diets of both males and females two years of age and older.52
Improving Dietary Magnesium Intake: Whole Foods
Dietary sources of magnesium include many whole foods, such as nuts, seeds, legumes, whole-grain cereals, and many vegetables (Table 3).53-57 Conversely, consumption of processed foods, sugars, saturated fats, and refined grains – all of which are common in the SAD – is associated with reduced intake of magnesium and other essential nutrients.58
Table 3. Dietary sources of magnesium.53-57
| Food group | Examples | Mg content (mg/100g) |
| Nuts and seeds | Pumpkin seeds | 592 |
| Flaxseed | 392 | |
| Sesame seeds | 356 | |
| Almonds | 270 | |
| Cashews | 260 | |
| Walnuts | 158 | |
| Pistachios | 109 | |
| Legumes | Peanuts | 178 |
| Soybeans | 86 | |
| Chickpeas | 48 | |
| Kidney beans | 45 | |
| Lentils | 36 | |
| Produce | Sun-dried tomatoes | 194 |
| Spinach | 87 | |
| Kale | 57 | |
| Dates | 54 | |
| Fresh parsley | 50 | |
| Potatoes with skin | 43 | |
| Whole grains | Buckwheat flour | 251 |
| Amaranth grain | 248 | |
| Quinoa grain | 197 | |
| Oats | 177 | |
| Spelt | 136 | |
| Barley | 133 | |
| Dairy | Parmesan cheese | 44 |
| Feta cheese | 19 | |
| Whole-fat milk | 13 | |
| Whole-fat yogurt | 12 | |
| Egg | 12 | |
| Seafood | Cod | |
| Salmon | ||
| Meat | Chicken breast | 34 |
| Turkey | 32 |
In a worrying trend, studies have described declining concentrations of micronutrients in food since the first half of the 20th century. For example, investigators have identified magnesium reductions of four percent to eight percent in beef, four percent in chicken, 38 percent in cheddar cheese, 70 percent in parmesan cheese, 21 percent in whole milk, and 24 percent in vegetables over decades.59 The magnesium content of wheat has dropped almost 20 percent since the 1960s, likely due to changes in the soil (e.g., acidification, mineral depletion) and modern cultivation practices (e.g., selective breeding, chemical fertilizers).60 The processing and refinement of food leads to further substantial losses of magnesium. In fact, most processed foods and highly refined grains (e.g., white flour, sugar) are essentially devoid of magnesium.
An analysis of NHANES data (2007-2010) suggested that even with adequate dairy intake (a common source of magnesium), magnesium deficiencies would remain highly prevalent in Americans (34 percent to 75 percent of males, 17 percent to 51 percent of females).5
Variety Matters
Magnesium levels vary by type of plant, cultivar, and plant anatomy. Magnesium is mobile in the phloem and can be found in high concentrations in rapidly growing structures with good access to phloem, such as roots, seeds, tubers, and fruit. Some species with higher concentrations of magnesium in the leaves include beets, chard, and spinach.61 Magnesium concentrations also vary by cultivar. One review identified magnesium levels ranging from 45.8 to 69.3 mg/100 g across varieties of kale and 8.7 to 12.3 mg/100 g among types of carrots.61
Given the wide range of magnesium levels within and between plants, consuming a variety of plants may be the best strategy to optimize dietary magnesium intake.
The Benefits of Magnesium Supplementation
With the declining levels of magnesium in available foods, many people may be challenged to maintain adequate magnesium levels through diet alone. Magnesium supplements are another option to support healthy magnesium status. Compared to food alone, the addition of dietary supplements significantly increases intake of nutrients, including magnesium, and reduces nutrient inadequacies in adults.62 The benefits of magnesium supplementation have been widely demonstrated. Several such studies are illustrated in Table 1. Additional studies have linked magnesium supplementation to reduced stress and depressive symptoms. For example, a study from France evaluated the effect of supplementation with magnesium, probiotics, and vitamins in 242 subjects with psychological stress.63 Following one month of supplementation, measures of subjects’ psychological stress decreased significantly (P<0.0001); fatigue scores also decreased significantly (P<0.0001). An open-label, randomized study evaluated the effect of magnesium supplementation in 126 adults with mild-to-moderate depression.64 After six weeks of magnesium chloride supplementation, depressive symptoms improved significantly over baseline (6.0 point improvement in Patient Health Questionnaire-9 scores, P<0.001). Anxiety scores also improved significantly. The supplement was well tolerated, and 61 percent of participants said they would use magnesium in the future.
Many people are in need of some level of magnesium supplementation. These deficits are illustrated in Table 4, which shows the mean daily intake of magnesium in the 2011-2012 NHANES survey compared to RDA.65 The addition of a supplement containing 100mg dietary magnesium would bring the mean magnesium intake to within the RDA values for both genders, for all age brackets.
Table 4. Magnesium intake from food and beverages compared to RDA and the impact of a 100 mg/day magnesium supplement. Data from the 2011-2012 NHANES survey.65
| Gender | Age (years) | Daily intake (mg/day) | RDA (mg/day) | Mg deficit (mg) | Difference with 100 mg/day supplement (mg) |
| Male | 20-29 | 346 | 400 | -54 | +46 |
| 30-39 | 388 | 420 | -32 | +68 | |
| 40-49 | 375 | 420 | -45 | +55 | |
| 50-59 | 348 | 420 | -72 | +28 | |
| 60-69 | 360 | 420 | -60 | +40 | |
| ≥70 | 301 | 420 | -119 | -19 | |
| Female | 20-29 | 266 | 310 | -44 | +66 |
| 30-39 | 299 | 320 | -21 | +79 | |
| 40-49 | 275 | 320 | -45 | +55 | |
| 50-59 | 278 | 320 | -42 | +58 | |
| 60-69 | 272 | 320 | -48 | +52 | |
| ≥70 | 249 | 320 | -71 | +29 |
Magnesium is an essential nutrient for human health. Deficiencies in magnesium increase risk for serious chronic diseases, whereas increased intake through improved diet and/or supplementation can improve health status and reduce disease risk. Unfortunately, current evidence indicates that half or more of Americans currently have some degree of subclinical magnesium deficiency. Increasing magnesium intake requires greater consumption of whole foods (unrefined grains, vegetables, fruits, nuts) and reduced intake of refined or processed foods. For many people, the addition of a magnesium supplement may be required to replete magnesium stores and maintain healthy magnesium levels over the long term.
- Grober, U., Schmidt, J., Kisters, K. (2015) Magnesium in prevention and therapy. Nutrients; 7(9):8199-8226.
- Volpe, SL. (2013). Magnesium in disease prevention and overall health. Adv Nutr; 4(3):378S-383S.
- Rosique-Esteban, N., Guasch-Ferre, M., Hernandez-Alonso, P., Salas-Salvado, J. (2018). Dietary magnesium and cardiovascular disease: a review with emphasis in epidemiological studies. Nutrients; 10(2).
- Elin, RJ. (2010). Assessment of magnesium status for diagnosis and therapy. Magnes Res; 23(4):S194-198.
- Quann, EE., Fulgoni, VL., Auestad, N. (2015). Consuming the daily recommended amounts of dairy products would reduce the prevalence of inadequate micronutrient intakes in the United States: diet modeling study based on NHANES 2007-2010. Nutr J. 14:90.
- Moshfegh, AG., Goldman, J., Ahuja, J., Rhodes, D., LaComb, R. (2009). What we eat in America, NHANES 2005-2006: usual nutrient intakes from food and water compared to 1997 dietary reference intakes for citamin D, calcium, phosphorus, and magneisum. Washington, DC: U.S. Department of Agriculture, Agriculture Research Service.
- Wang, JL., Shaw, NS., Yeh, HY., Kao, MD. (2005). Magnesium status and association with diabetes in the Taiwanese elderly. Asia Pac J Clin Nutr;14(3):263-269.
- Olza, J., Aranceta-Bartrina, J., Gonzalez-Gross, M., et al. (2017). Reported dietary intake, disparity between the reported consumption and the level needed for adequacy and food sources of calcium, phosphorus, magnesium and vitamin D in the Spanish population: findings from the ANIBES study. Nutrients; 9(2).
- Costello, RB., Elin, RJ., Rosanoff, A., et al.(2016). Perspective: The case for an evidence-based reference interval for serum magnesium: the time has come. Adv Nutr.; 7(6):977-993.
- Vormann, J. (2003). Magnesium: nutrition and metabolism. Mol Aspects Med; 24(1-3):27-37.
- Jahnen-Dechent, W., Ketteler, M. (2012). Magnesium basics. Clin Kidney J;5 (Suppl 1):i3-i14.
- Rude, RK., Gruber, HE. (2004). Magnesium deficiency and osteoporosis: animal and human observations. J Nutr Biochem; 15(12):710-716.
- Nielsen, FH., Milne, DB., Gallagher, S., Johnson, L., Hoverson, B. (2007). Moderate magnesium deprivation results in calcium retention and altered potassium and phosphorus excretion by postmenopausal women. Magnes Res; 20(1):19-31.
- Schwalfenberg GK., Genuis, SJ. (2017). The Importance of magnesium in clinical healthcare. Scientifica (Cairo):4179326.
- Hermes Sales, C., Azevedo Nascimento, D., Queiroz Medeiros, AC., Costa Lima, K., Campos Pedrosa, LF., Colli, C. (2014). There is chronic latent magnesium deficiency in apparently healthy university students. Nutr Hosp; 30(1):200-204.
- Elin, RJ. (2011). Re-evaluation of the concept of chronic, latent, magnesium deficiency. Magnes Res; 24(4):225-227.
- Mejia-Rodriguez, F., Shamah-Levy, T., Villalpando, S., Garcia-Guerra, A., Mendez-Gomez Humaran, I. (2013). Iron, zinc, copper and magnesium deficiencies in Mexican adults from the National Health and Nutrition Survey 2006. Salud Publica Mex.; 55(3):275-284.
- DiNicolantonio, JJ., O’Keefe, JH., Wilson, W. (2018). Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart; 5(1):e000668.
- Kunutsor, SK., Whitehouse, MR., Blom, AW., Laukkanen, JA. (2017). Low serum magnesium levels are associated with increased risk of fractures: a long-term prospective cohort study. Eur J Epidemiol; 32(7):593-603.
- Orchard, TS., Larson, JC., Alghothani, N., et al. (2014). Magnesium intake, bone mineral density, and fractures: results from the women’s health initiative observational study. Am J Clin Nutr; 99(4):926-933.
- Rude, RK., Singer, FR., Gruber, HE. (2009). Skeletal and hormonal effects of magnesium deficiency. J Am Coll Nutr.;28(2):131-141.
- Mahdavi-Roshan, M., Ebrahimi, M., Ebrahimi, A. (2015). Copper, magnesium, zinc and calcium status in osteopenic and osteoporotic post-menopausal women. Clin Cases Miner Bone Metab.12(1):18-21.
- Szkup, M., Jurczak, A., Brodowska, A., et al. (2017). Analysis of relations between the level of Mg, Zn, Ca, Cu, and Fe and depressiveness in postmenopausal women. Biol Trace Elem Res;176(1):56-63.
- Rajizadeh, A., Mozaffari-Khosravi, H., Yassini-Ardakani, M., Dehghani, A. (2017). Effect of magnesium supplementation on depression status in depressed patients with magnesium deficiency: A randomized, double-blind, placebo-controlled trial. Nutrition; 35:56-60.
- Taveira, TH., Ouellette, D., Gulum, A., et al. (2016). Relation of Magnesium intake with cardiac function and heart failure hospitalizations in black adults: the jackson heart study. Circ Heart Fail;9(4):e002698.
- Fang, X., Wang, K., Han, D., et al. (2018).Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med; 14(1):210.
- Han, H., Fang, X., Wei, X., et al. (2017). Dose-response relationship between dietary magnesium intake, serum magnesium concentration and risk of hypertension: a systematic review and meta-analysis of prospective cohort studies. Nutr J; 16(1):26.
- Dibaba, DT., Xun, P., Song, Y., Rosanoff, A., Shechter, M., He, K. (2017). The effect of magnesium supplementation on blood pressure in individuals with insulin resistance, prediabetes, or noncommunicable chronic diseases: a meta-analysis of randomized controlled trials. Am J Clin Nutr; 106(3):921-929.
- Zhang, X., Li, Y., Del Gobbo, LC., et al. (2016). Effects of magnesium supplementation on blood pressure: A meta-analysis of randomized double-blind placebo-controlled trials. Hypertension; 68(2):324-333.
- Rebholz, CM. Tin, A., Liu, Y., et al.(2016). Dietary magnesium and kidney function decline: the healthy aging in neighborhoods of diversity across the life span study. Am J Nephrol;44(5):381-387.
- Sarrafzadegan, N., Khosravi-Boroujeni, H., Lotfizadeh, M., Pourmogaddas, A., Salehi-Abargouei, A. (2016). Magnesium status and the metabolic syndrome: A systematic review and meta-analysis. Nutrition; 32(4):409-417.
- He, K., Liu, K., Daviglus, ML., et al. (2006). Magnesium intake and incidence of metabolic syndrome among young adults. Circulation; 113(13):1675-1682.
- Hruby, A., Meigs, JB., O’Donnell, CJ., Jacques, PF., McKeown, NM. (2014). Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged americans. Diabetes Care; 37(2):419-427.
- Simental-Mendia, LE., Sahebkar, A., Rodriguez-Moran, M., Guerrero-Romero, F. (2016). A systematic review and meta-analysis of randomized controlled trials on the effects of magnesium supplementation on insulin sensitivity and glucose control. Pharmacol Res; 111:272-282.
- Tarighat Esfanjani, A., Mahdavi, R., Ebrahimi Mameghani, M., Talebi, M., Nikniaz, Z., Safaiyan, A. (2012). The effects of magnesium, L-carnitine, and concurrent magnesium-L-carnitine supplementation in migraine prophylaxis. Biol Trace Elem Res; 150(1-3):42-48.
- Adebamowo, SN., Spiegelman, D., Willett, WC., Rexrode, KM. (2015). Association between intakes of magnesium, potassium, and calcium and risk of stroke: 2 cohorts of US women and updated meta-analyses. Am J Clin Nutr.; 101(6):1269-1277.
- Fang, X., Han, H., Li, M., et al. (2016). Dose-response relationship between dietary Magnesium Intake and Risk of Type 2 Diabetes Mellitus: A Systematic Review and meta-regression analysis of prospective cohort studies. Nutrients; 8(11).
- Hruby, A., Guasch-Ferre, M., Bhupathiraju, SN., et al. (2017). Magnesium intake, quality of carbohydrates, and risk of type 2 diabetes: results from three U.S. cohorts. Diabetes Care; 40(12):1695-1702.
- Guerrero-Romero, F., Simental-Mendia, LE., Hernandez-Ronquillo, G., Rodriguez-Moran, M. (2015). Oral magnesium supplementation improves glycaemic status in subjects with prediabetes and hypomagnesaemia: A double-blind placebo-controlled randomized trial. Diabetes Metab; 41(3):202-207.
- Hayhoe, RPG., Lentjes, MAH., Mulligan, AA., Luben, RN., Khaw, KT., Welch, AA. (2018). Cross-sectional associations of dietary and circulating magnesium with skeletal muscle mass in the EPIC-Norfolk cohort. Clin Nutr.
- Veronese, N., Stubbs, B., Maggi, S., et al. (2017). Dietary magnesium and incident frailty in older people at risk for knee osteoarthritis: an eight-year longitudinal study. Nutrients; 9(11).
- Welch, AA., Skinner, J., Hickson, M. (2017). Dietary magnesium may be protective for aging of bone and skeletal muscle in middle and younger older age men and women: cross-sectional findings from the UK biobank cohort. Nutrients; 9(11).
- Wu, L., Zhu, X., Fan, L., et al. (2017). Magnesium intake and mortality due to liver diseases: Results from the third national health and nutrition examination survey cohort. Sci Rep; 7(1):17913.
- Wakimoto, P., Block, G.(2001). Dietary intake, dietary patterns, and changes with age: an epidemiological perspective. J Gerontol A Biol Sci Med Sci; 56 Spec No 2:65-80.
- Killilea, DW., Maier, JA. (2008). A connection between magnesium deficiency and aging: new insights from cellular studies. Magnes Res; 21(2):77-82.
- Lin, J., Epel, E., Blackburn, E. (2012). Telomeres and lifestyle factors: roles in cellular aging. Mutat Res; 730(1-2):85-89.
- Mazidi, M., Kengne, AP., Banach, M. (2017). Mineral and vitamin consumption and telomere length among adults in the United States. Pol Arch Intern Med.; 127(2):87-90.
- Shah, NC., Shah, GJ., Li, Z., Jiang, XC., Altura, BT., Altura, BM. (2014). Short-term magnesium deficiency downregulates telomerase, upregulates neutral sphingomyelinase and induces oxidative DNA damage in cardiovascular tissues: relevance to atherogenesis, cardiovascular diseases and aging. Int J Clin Exp Med; 7(3):497-514.
- Kunutsor, SK., Whitehouse, MR., Blom, AW., Laukkanen, JA. (2017). Low serum magnesium levels are associated with increased risk of fractures: a long-term prospective cohort study. Eur J Epidemiol; 32(7):593-603.
- Orchard, TS., Larson, JC., Alghothani, N., et al. (2014). Magnesium intake, bone mineral density, and fractures: results from the women’s health initiative observational study. Am J Clin Nutr; 99(4):926-933.
- Rude, RK., Singer, FR., Gruber, HE. (2009). Skeletal and hormonal effects of magnesium deficiency. J Am Coll Nutr.;28(2):131-141.
- Mahdavi-Roshan, M., Ebrahimi, M., Ebrahimi, A. (2015). Copper, magnesium, zinc and calcium status in osteopenic and osteoporotic post-menopausal women. Clin Cases Miner Bone Metab.12(1):18-21.
- Szkup, M., Jurczak, A., Brodowska, A., et al. (2017). Analysis of relations between the level of Mg, Zn, Ca, Cu, and Fe and depressiveness in postmenopausal women. Biol Trace Elem Res;176(1):56-63.
- Rajizadeh, A., Mozaffari-Khosravi, H., Yassini-Ardakani, M., Dehghani, A. (2017). Effect of magnesium supplementation on depression status in depressed patients with magnesium deficiency: A randomized, double-blind, placebo-controlled trial. Nutrition; 35:56-60.
- Taveira, TH., Ouellette, D., Gulum, A., et al. (2016). Relation of Magnesium intake with cardiac function and heart failure hospitalizations in black adults: the jackson heart study. Circ Heart Fail;9(4):e002698.
- Fang, X., Wang, K., Han, D., et al. (2018).Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med; 14(1):210.
- Han, H., Fang, X., Wei, X., et al. (2017). Dose-response relationship between dietary magnesium intake, serum magnesium concentration and risk of hypertension: a systematic review and meta-analysis of prospective cohort studies. Nutr J; 16(1):26.
- Dibaba, DT., Xun, P., Song, Y., Rosanoff, A., Shechter, M., He, K. (2017). The effect of magnesium supplementation on blood pressure in individuals with insulin resistance, prediabetes, or noncommunicable chronic diseases: a meta-analysis of randomized controlled trials. Am J Clin Nutr; 106(3):921-929.
- Zhang, X., Li, Y., Del Gobbo, LC., et al. (2016). Effects of magnesium supplementation on blood pressure: A meta-analysis of randomized double-blind placebo-controlled trials. Hypertension; 68(2):324-333.
- Rebholz, CM. Tin, A., Liu, Y., et al.(2016). Dietary magnesium and kidney function decline: the healthy aging in neighborhoods of diversity across the life span study. Am J Nephrol;44(5):381-387.
- Sarrafzadegan, N., Khosravi-Boroujeni, H., Lotfizadeh, M., Pourmogaddas, A., Salehi-Abargouei, A. (2016). Magnesium status and the metabolic syndrome: A systematic review and meta-analysis. Nutrition; 32(4):409-417.
- He, K., Liu, K., Daviglus, ML., et al. (2006). Magnesium intake and incidence of metabolic syndrome among young adults. Circulation; 113(13):1675-1682.
- Hruby, A., Meigs, JB., O’Donnell, CJ., Jacques, PF., McKeown, NM. (2014). Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged americans. Diabetes Care; 37(2):419-427.
- Simental-Mendia, LE., Sahebkar, A., Rodriguez-Moran, M., Guerrero-Romero, F. (2016). A systematic review and meta-analysis of randomized controlled trials on the effects of magnesium supplementation on insulin sensitivity and glucose control. Pharmacol Res; 111:272-282.
- Tarighat Esfanjani, A., Mahdavi, R., Ebrahimi Mameghani, M., Talebi, M., Nikniaz, Z., Safaiyan, A. (2012). The effects of magnesium, L-carnitine, and concurrent magnesium-L-carnitine supplementation in migraine prophylaxis. Biol Trace Elem Res; 150(1-3):42-48.
- Adebamowo, SN., Spiegelman, D., Willett, WC., Rexrode, KM. (2015). Association between intakes of magnesium, potassium, and calcium and risk of stroke: 2 cohorts of US women and updated meta-analyses. Am J Clin Nutr.; 101(6):1269-1277.
- Fang, X., Han, H., Li, M., et al. (2016). Dose-response relationship between dietary Magnesium Intake and Risk of Type 2 Diabetes Mellitus: A Systematic Review and meta-regression analysis of prospective cohort studies. Nutrients; 8(11).
- Hruby, A., Guasch-Ferre, M., Bhupathiraju, SN., et al. (2017). Magnesium intake, quality of carbohydrates, and risk of type 2 diabetes: results from three U.S. cohorts. Diabetes Care; 40(12):1695-1702.
- Guerrero-Romero, F., Simental-Mendia, LE., Hernandez-Ronquillo, G., Rodriguez-Moran, M. (2015). Oral magnesium supplementation improves glycaemic status in subjects with prediabetes and hypomagnesaemia: A double-blind placebo-controlled randomized trial. Diabetes Metab; 41(3):202-207.
- Hayhoe, RPG., Lentjes, MAH., Mulligan, AA., Luben, RN., Khaw, KT., Welch, AA. (2018). Cross-sectional associations of dietary and circulating magnesium with skeletal muscle mass in the EPIC-Norfolk cohort. Clin Nutr.
- Veronese, N., Stubbs, B., Maggi, S., et al. (2017). Dietary magnesium and incident frailty in older people at risk for knee osteoarthritis: an eight-year longitudinal study. Nutrients; 9(11).
- Welch, AA., Skinner, J., Hickson, M. (2017). Dietary magnesium may be protective for aging of bone and skeletal muscle in middle and younger older age men and women: cross-sectional findings from the UK biobank cohort. Nutrients; 9(11).
- Wu, L., Zhu, X., Fan, L., et al. (2017). Magnesium intake and mortality due to liver diseases: Results from the third national health and nutrition examination survey cohort. Sci Rep; 7(1):17913.
- Wakimoto, P., Block, G.(2001). Dietary intake, dietary patterns, and changes with age: an epidemiological perspective. J Gerontol A Biol Sci Med Sci; 56 Spec No 2:65-80.
- Killilea, DW., Maier, JA. (2008). A connection between magnesium deficiency and aging: new insights from cellular studies. Magnes Res; 21(2):77-82.
- Lin, J., Epel, E., Blackburn, E. (2012). Telomeres and lifestyle factors: roles in cellular aging. Mutat Res; 730(1-2):85-89.
- Mazidi, M., Kengne, AP., Banach, M. (2017). Mineral and vitamin consumption and telomere length among adults in the United States. Pol Arch Intern Med.; 127(2):87-90.
- Shah, NC., Shah, GJ., Li, Z., Jiang, XC., Altura, BT., Altura, BM. (2014). Short-term magnesium deficiency downregulates telomerase, upregulates neutral sphingomyelinase and induces oxidative DNA damage in cardiovascular tissues: relevance to atherogenesis, cardiovascular diseases and aging. Int J Clin Exp Med; 7(3):497-514.







